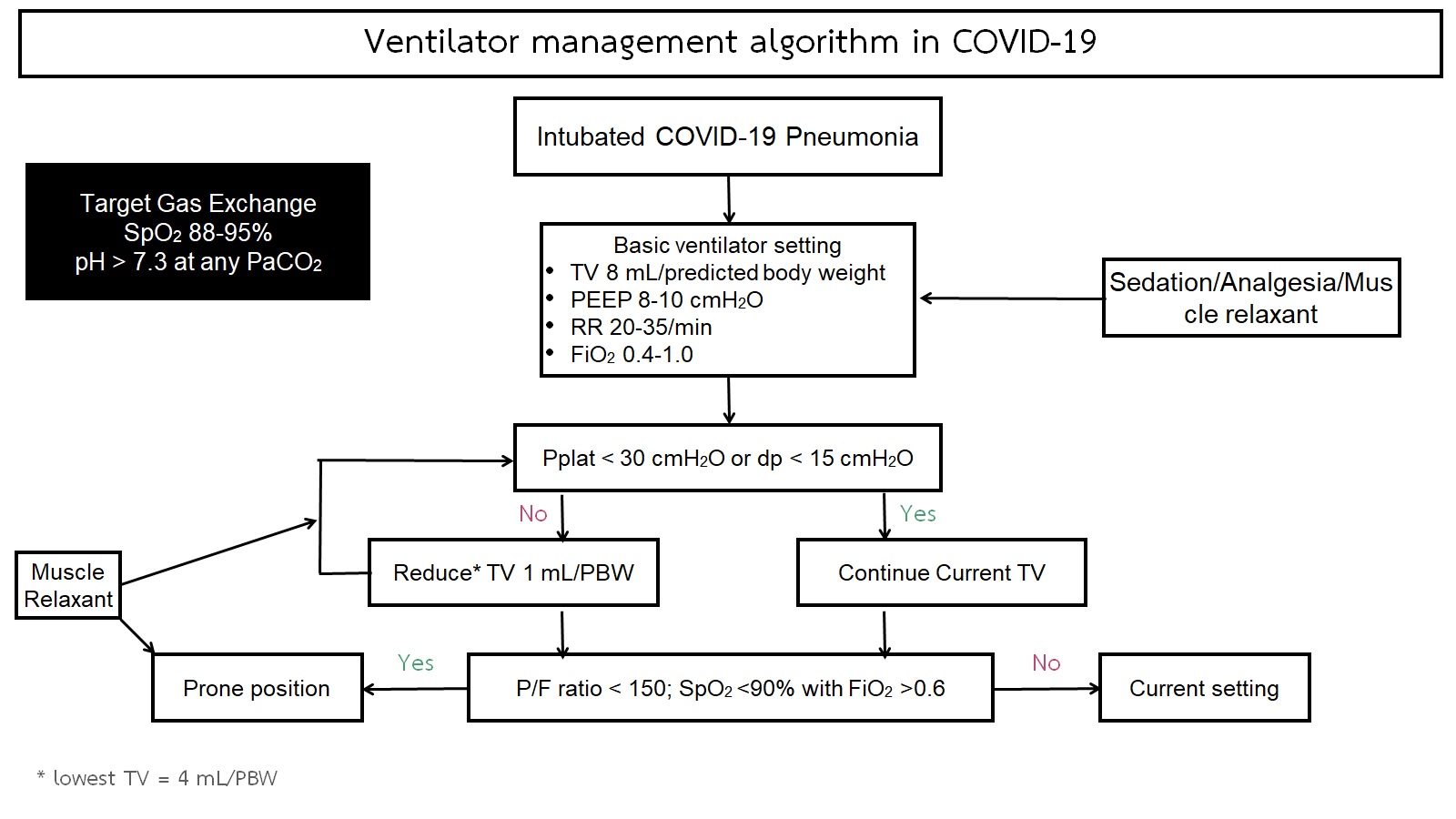
Mechanical ventilator support and prone positioning in COVID-19 related pneumonia
Mechanical ventilator support in COVID-19
Keywords:
COVID-19, CARDS, Prone positioning, Mechanical ventilatorAbstract
COVID-19 is currently a global pandemic that cause high morbidity and mortality, particularly in the critical cases. The common presentation is among the common respiratory symptoms and could be deteriorated to multiple organ failure. From the previous epidemiologic study, approximate 15% of cases developed pneumonia and 5% required intensive care admission. The optimal respiratory care including oxygen support are the key for hypoxic respiratory failure from severe COVID-19. Several devices have been practically suggested for respiratory symptoms included high flow nasal cannula (HFNC), non-invasive positive pressure ventilator (NIV) via either common facial mask or helmet. However, some patients did not improve with those devices, that become more respiratory distress and eventually required intubation and mechanical ventilator support. In this brief review, the author will pay attention on the mechanical ventilator support and prone positioning for COVID-19 pneumonia.
Downloads
References
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020, 382(18):1708-1720.
Namendys-Silva SA. Respiratory support for patients with COVID-19 infection. Lancet Respir Med 2020, 8(4):e18.
King CS, Sahjwani D, Brown AW, Feroz S, Cameron P, Osborn E, et al. Outcomes of mechanically ventilated patients with COVID-19 associated respiratory failure. PLoS One 2020, 15(11):e0242651.
Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med 2020, 46(6):1099-1102.
Tobin MJ. Basing Respiratory Management of COVID-19 on Physiological Principles. American Journal of Respiratory and Critical Care Medicine 2020, 201(11):1319-1320.
Gorman E, Connolly B, Couper K, Perkins GD, McAuley DF. Non-invasive respiratory support strategies in COVID-19. Lancet Respir Med 2021.
Papoutsi E, Giannakoulis VG, Xourgia E, Routsi C, Kotanidou A, Siempos II. Effect of timing of intubation on clinical outcomes of critically ill patients with COVID-19: a systematic review and meta-analysis of non-randomized cohort studies. Crit Care 2021, 25(1):121.
Bayrak V, Senturk Durukan N, Demirer Aydemir F, Ergan B, Gezer NS, Eren Kutsoylu OO, et al. Risk Factors Associated with Mortality in Intensive Care COVID-19 Patients: the importance of chest CT score and intubation timing as risk factors. Turk J Med Sci 2021.
Luo M, Cao S, Wei L, Zhao X, Gao F, Li S, et al. Intubation, mortality, and risk factors in critically ill Covid-19 patients: A pilot study. J Clin Anesth 2020, 67:110039.
Chandel A, Patolia S, Brown AW, Collins AC, Sahjwani D, Khangoora V, et al. High-Flow Nasal Cannula Therapy in COVID-19: Using the ROX Index to Predict Success. Respir Care 2021, 66(6):909-919.
Apigo M, Schechtman J, Dhliwayo N, Al Tameemi M, Gazmuri RJ. Development of a work of breathing scale and monitoring need of intubation in COVID-19 pneumonia. Crit Care 2020, 24(1):477.
Orser BA. Recommendations for Endotracheal Intubation of COVID-19 Patients. Anesth Analg 2020, 130(5):1109-1110.
Marini JJ, Gattinoni L. Management of COVID-19 Respiratory Distress. JAMA 2020, 323(22):2329-2330.
Lee WL, Detsky AS, Stewart TE. Lung-protective mechanical ventilation strategies in ARDS. Intensive Care Med 2000, 26(8):1151-1155.
Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med 2016, 42(10):1567-1575.
Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome. New England Journal of Medicine 2000, 342(18):1301-1308.
Cruces P, Donoso A, Valenzuela J, Diaz F. Respiratory and hemodynamic effects of a stepwise lung recruitment maneuver in pediatric ARDS: a feasibility study. Pediatr Pulmonol 2013, 48(11):1135-1143.
Stevic N, Chatelain E, Dargent A, Argaud L, Cour M, Guerin C. Lung Recruitability Evaluated by Recruitment-to-Inflation Ratio and Lung Ultrasound in COVID-19 Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med 2021, 203(8):1025-1027.
Chen L, Del Sorbo L, Grieco DL, Junhasavasdikul D, Rittayamai N, Soliman I, et al. Potential for Lung Recruitment Estimated by the Recruitment-to-Inflation Ratio in Acute Respiratory Distress Syndrome. A Clinical Trial. Am J Respir Crit Care Med 2020, 201(2):178-187.
Povoa P, Almeida E, Fernandes A, Mealha R, Moreira P, Sabino H. Evaluation of a recruitment maneuver with positive inspiratory pressure and high PEEP in patients with severe ARDS. Acta Anaesthesiol Scand 2004, 48(3):287-293.
Honore PM, Mugisha A, Kugener L, Redant S, Attou R, Gallerani A, et al. The use of a neuromuscular blocking agent could significantly decrease mortality in moderate-to-severe ARDS patients: is moderate ARDS the best indication for neuromuscular blocking agents. Crit Care 2020, 24(1):217.
Gattinoni L, Busana M, Giosa L, Macri MM, Quintel M. Prone Positioning in Acute Respiratory Distress Syndrome. Semin Respir Crit Care Med 2019, 40(1):94-100.
Guerin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013, 368(23):2159-2168.
Thompson AE, Ranard BL, Wei Y, Jelic S. Prone Positioning in Awake, Nonintubated Patients With COVID-19 Hypoxemic Respiratory Failure. JAMA Intern Med 2020, 180(11):1537-1539.
Damarla M, Zaeh S, Niedermeyer S, Merck S, Niranjan-Azadi A, Broderick B, et al. Prone Positioning of Nonintubated Patients with COVID-19. Am J Respir Crit Care Med 2020, 202(4):604-606.
Elharrar X, Trigui Y, Dols AM, Touchon F, Martinez S, Prud’homme E, et al. Use of Prone Positioning in Nonintubated Patients With COVID-19 and Hypoxemic Acute Respiratory Failure. JAMA 2020, 323(22):2336-2338.
Weatherald J, Solverson K, Zuege DJ, Loroff N, Fiest KM, Parhar KKS. Awake prone positioning for COVID-19 hypoxemic respiratory failure: A rapid review. J Crit Care 2021, 61:63-70.
Rahmani F, Salmasi S, Rezaeifar P. Prone Position Effects in the Treatment of Covid-19 Patients. Caspian J Intern Med 2020, 11(Suppl 1):580-582.