Physiologic cardiovascular studies among patients with treated septic shock and persistent hyperlactatemia
Keywords:
Sepsis, Ventriculo-arterial coupling, Venous return, LactateAbstract
Background: To study effects of increasing vasopressor dosage and fluid resuscitation on ventriculoarterial (VA) coupling and venous return (VR)-related parameters in resuscitated normotensive septic shock patients with persistent hyperlactatemia.
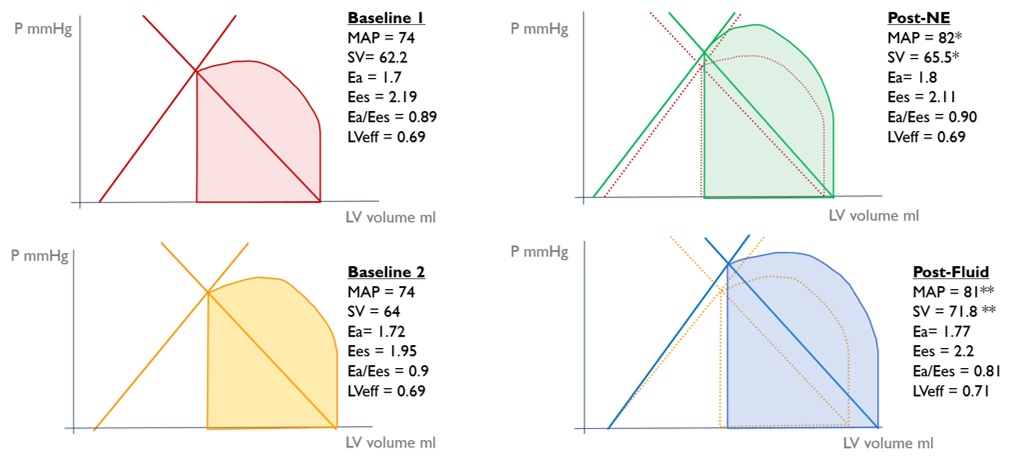
Methods: We performed a prospective experimental study in patients with septic shock who was admitted to medical intensive care unit and still had hyperlactatemia even received initial resuscitation to maintain mean arterial pressure (MAP) >65 mmHg. All patients received incremental dose of norepinephrine (NE) to increased MAP, then NE was titrated to baseline dosage and waited for 15 mins, then fluid bolus was given. VA coupling-related parameters [arterial elastance (Ea), left ventricular end-systolic elastance (Ees), left ventricular stroke work (SW), potential energy (PE), stroke volume (SV), and Ea/Ees], and VR-related parameters [central venous pressure (CVP), mean systemic pressure analogue (Pmsa), venous return pressure (Pvr)] were measured at 4 time points including pre-increased NE phase, post-increased NE phase, pre-fluid bolus phase, and post-fluid bolus phase. Primary outcome was average of Ea/Ees. Secondary outcomes were differences in VA coupling-related parameters and VR-related parameters between pre- vs. post- interventions.
Results: All 20 patients were normotensive [MAP 74 (66-80) mmHg] with elevated blood lactate [2.7 (2.4-3.6) mmol/L] at enrollment. Average Ea/Ees was 0.89 (0.61-1.16). Compared to pre-increased NE phase, post-increased NE phase had significantly higher MAP, CVP, SV, SW, PE, Pmsa, and Pvr. Likewise, compared to pre-fluid bolus phase, post-fluid bolus raised MAP, CVP, SV, Ees, SW, Pmsa, and Pvr significantly. No difference in Ea/Ees compared between before- vs. after- received both interventions.
Conclusions: In resuscitated normotensive septic shock patients with persistent hyperlactatemia, we found an average Ea/Ees of 0.89. Increasing NE dosage or fluid bolus increased most of VA coupling-related parameters and VR-related parameters, but not Ea/Ees. Further large study is warranted to validate these findings.
Downloads
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801-10
Cecconi M, Evans L, Levy M, Rhodes A. Sepsis and septic shock. Lancet. 2018; 392:75-87.
Vincent JL, Marshall JC, Namendys-Silva SA, François B, Martin-Loeches I, Lipman J, et al. Assessment of the worldwide burden of critical illness. the intensive cate over nations (ICON) audit. Lancet Respir Med. 2014;2:380-6.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Survival sepsis campaign: international guidelines for management of sepsis and septic shock:2016 Intensive Care Med. 2017;43:304-77.
Yan J, Zhou X, Hu B, Gong S, Yu Y, Cai G, Li L. Prognostic value of left ventricular-arterial coupling in elderly patients with septic shock. J Crit Care. 2017;42:289-293.
Suzuki T, Suzuki Y, Okuda J, Kurazumi T, Suhara T, Ueda T, et al. Sepsis-induced cardiac dysfunction and B-adrenergic blockade therapy for sepsis. J Intensive Care. 2017;5:22.
Parillo JE, Packer MM, Natanson C, Suffredini AF, Danner RL, Cunnion RE, et al. Septic shock in humans. Advances in the understanding of pathogenesis, cardiovascular dysfunction, and therapy. Ann Intern Med. 1990;113:227-42.
Charpentier J, Luyt CE, Fulla Y, Vinsonneau C, Cariou A, Grabar S, et al. Brain natriuretic peptide: a marker of myocardial dysfunction and prognosis during severe sepsis. Crit Care Med. 2004;32:660-5.
Guarracino F, Baldassarri R, Pinsky MR. Ventriculo-arterial decoupling in acutely altered hemodynamic states. Crit Care. 2013;17:213.
Guarracino F, Bertini P, Pinsky MR. Cardiovascular determinants of resuscitation from sepsis and septic shock. Crit Care. 2019;23:118.
Maas JJ, Geerts BF, de Wilde RB, Pinsky MR, Jansen JR. Assessment of venous return curve and mean systemic filling pressure in post-operative cardiac surgery patients. Crit Care Med. 2009;37:912-8.
Parkin WG, Leaning MS. Therapeutic control of the circulation. J Clin Monit Comput. 2008;22:391-400.
Pinsky MR, Guarracino F. How to assess ventriculoarterial coupling in sepsis. Curr Opin Crit Care. 2020;26:313-318.
Elzinga G, Westerhof N. Matching between ventricle and arterial load. Circ Res. 1991;68:1495–1500.
Kass DA, Kelly RP. Ventriculo-arterial coupling: concepts, assumptions, and applications. Ann Biomed Eng. 1992;20:41–62.
Pinsky MR. Both perfusion pressure and flow are essential for adequate resuscitation. Sepsis 2001;4:143-146.
Canterin FA, Poli S, Vritz O, Pavan D, Bello VD, Nicolosi GL. The ventricular-arterial coupling: from basic pathophysiology to clinical application in the echocardiography laboratory. J Cardiovasc Echogr. 2013;23(4):91-95.
Garcia MM, Santos A. Understanding ventriculo-arterial coupling. Ann Transl Med. 2020;8:795.
Chen CH, Fetics B, Nevo E, Rochitte CE, Chiou KR, Ding PA, et al. Noninvasive single-beat determination of left ventricular end-systolic elastance in humans. J Am Coll Cardiol. 2001;38:2028-34.
Wiginberge M, Sindhunata DP, Pinsky M, Vlaar AP, Ouweneel E, Jansen JR, et al. Estimating mean circulatory filling pressure in clinical practice: a systematic review comparing three bedside methods in the critically ill. Ann Intensive Care. 2018;8:73.
Vincent JL, Jones G, David S, Olariu E, Cadwell KK. Frequency and mortality of septic shock in Europe and North America: a systematic review and meta-analysis. Crit Care. 2019;23:196.
Jones AE. Lactate clearance for assessing response to resuscitation in severe sepsis. Acad Emerg Med. 2013;20:844-847.
Chantler PD, Lakatta EG, Najjar SS. Arterial-ventricular coupling: mechanistic insights into cardiovascular performance at rest and during exercise. J Appl Physiol. 2008;105:1342-1351.
Guarracino F, Ferro B, Moreeli A, Bertini P, Baldassarri R, Pinsky MR. Ventriculoarterial decoupling in human septic shock. Crit Care. 2014;18:R80.
Wang F, Zhang M, Wang X, Xiaopeng Z, Po D. Effects of norepinephrine on hemodynamics, vascular elasticity, cardiac pump function, and inflammatory factors in patients with septic shock. Eur J Inflamm. 2019;17:205873921983839.
Monnet X, Jabot J, Maizel J, Richard C, Teboul JL. Norepinephrine increases cardiac preload and reduces preload dependency assessed by passive leg raising in septic shock patients. Crit Care Med. 2011;39:689-94.
Persichini R, Silva S, Teboul JL, Jozwiak M, Chemla D, Richard C, et al. Effects of norepinephrine on mean systemic pressure and venous return in human septic shock. Crit Care Med. 2012;40:3146-3153.
Foulon P, Backer DD. The hemodynamic effects of norepinephrine: far more than an increase in blood pressure. Ann Transl Med. 2018;6(Suppl1):S25.
Marik P, Bellomo R. A rational approach to fluid therapy in sepsis. Br J Anasth. 2016;116:339-49.
Silverman HJ, Penaranda R, Orens JB, Lee NH. Impaired beta-adrenergic receptor stimulation of cyclic adenosine monophosphate in human septic shock: association with myocardial hyporesponsiveness to cathecholamines. Crit Care Med. 1993;21:31-9.
Chen CH, Nakayama M, Nevo E, Fetics BJ, Maughan WL, Kass DA. Coupled systolic-ventricular and vascular stiffening with age implications for pressure regulation and cardiac reserve in the elderly. JACC. 1998;32(5):1221-7.