Effect of adjunctive corticosteroid therapy on outcomes in pulmonary tuberculosis patients with acute respiratory failure: a cohort study
Steroid in tuberculosis respiratory failure
DOI:
https://doi.org/10.54205/ccc.v29.253581Keywords:
Adjunctive corticosteroid therapy, Outcomes, Pulmonary tuberculosis, Acute respiratory failureAbstract
Background: Tuberculosis (TB) remains an important and evolving health problem worldwide. Acute respiratory failure, the most severe form of pulmonary tuberculosis, is associated with a high mortality rate. Adjunctive corticosteroid therapy has been reported as an effective treatment in extrapulmonary TB. The aim of this study was to investigate the effect of adjunctive corticosteroid therapy on outcomes in pulmonary tuberculosis patients with acute respiratory failure.
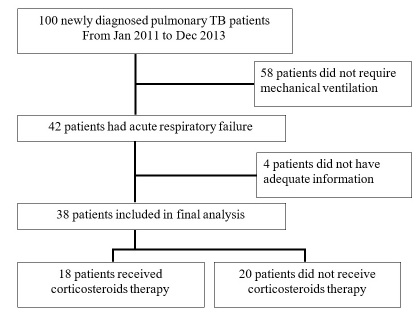
Methods: This retrospective cohort study enrolled newly diagnosed pulmonary tuberculosis patients with acute respiratory failure who were admitted to Siriraj Hospital (Bangkok, Thailand) during January 2011 to December 2013. Patients that received corticosteroid as an adjunctive treatment for pulmonary TB were assigned to the steroid group. The control group consisted of patients that did not receive corticosteroid. Collected data included age, gender, body mass index (BMI), Acute Physiology and Chronic Health Evaluation II (APACHE II) scores, sequential organ failure assessment (SOFA) scores, vital signs, PaO2/FiO2 ratio, chest X-ray abnormality pattern, and TB treatment strategies, including antituberculosis agents and adjunct corticosteroid treatment. The primary outcome was hospital mortality rate. The secondary outcomes were hospital length of stay and duration of mechanical ventilation.
Results: Thirty-eight patients were included. There were 18 patients in the steroid group and 20 in the control group. No significant difference was observed between groups for age, gender, BMI, APACHE II score, vital signs, or PaO2/FiO2 ratio. Patients in the steroid group had a significantly higher mean SOFA score than controls (5.7±4.5 vs. 3.3±2.6, respectively; p=0.046). Almost all patients in this study (97.1%) had positive culture for M. tuberculosis from sputum. The mean corticosteroid dose was equivalent to hydrocortisone 329.7±146.0 mg/day. Patients in the steroid group had higher hospital mortality than control group patients, but the difference did not achieve statistical significance (66.7% vs. 45.0%, respectively; p=0.21). Adjunctive corticosteroid therapy did not significantly reduce hospital length of stay or duration of mechanical ventilation when compared between the steroid and control groups (12.0±13.3 vs. 14.6±19.3 days, respectively; p=0.636 and 7.2±10.6 vs. 8.0±8.3 days, respectively; p=0.801).
Conclusion: Adjunctive corticosteroid therapy had no significant positive effect on outcomes in pulmonary tuberculosis patients with acute respiratory failure.
Downloads
References
World Health Organization, Global Tuberculosis Report 2016.
Frame RN, Johnson MC, Eichenhorn MS, Bower GC, Popovich JM Jr. Active tuberculosis in the medical intensive care unit: A 15-year retrospective analysis. Crit Care Med. 1987; 15:1012–4.
Silva DR, Menegotto DM, Schulz LF, Gazzana MB, Dalcin PT. Mortality among patients with tuberculosis requiring intensive care: a retrospective cohort study. BMC Infectious Diseases. 2010;10:54.
Levy H, Kallenbach JM, Feldman C, Thorburn JR, Abramowitz JA. Acute respiratory failure in active tuberculosis. Crit Care Med. 1987;15:221–5.
Agarwal MK, Muthuswamy PP, Shah RS, Addington WW. Respiratory failure in pulmonary tuberculosis. Chest. 1977;72:605-9.
Agarwal R, Gupta D, Aggarwal AN, Behera D, Jindal SK. Experience with ARDS caused by tuberculosis in a respiratory intensive care unit. Intensive Care Med. 2005;31:1284-7.
Kim JY, Park YB, Kim YS, Kang SB, Shin JW, Park IW, et al. Miliary tuberculosis and acute respiratory distress syndrome. Int J Tuberc Lung Dis. 2003;7:359-64.
Penner C, Roberts D, Kunimoto D, Manfreda J, Long R. Tuberculosis as a primary cause of respiratory failure requiring mechanical ventilation. Am J Respir Crit Care Med. 1995;151:867-72.
Anekrhananon T, Ratanasuwan W, Techasathit W, Suwanagool S,Dhiraputra C. Multidrug resistant Mycobacterium tuberculosis infections in patients with acquired immunodeficiency syndrome at Siriraj hospital. Siriraj Hosp Gaz. 2002;54:108-14.
Didonato JA, Saatcioglu F, Karin M. Molecular mechanisms of immunosuppression and anti-inflammatory activities by glucocorticoids. Am J Respir Crit Care Med. 1996;154:511-5.
Thwaites GE, Nguyen DB, Nguyen HD, Hoang TQ, Do TT, Nguyen TC, et al. Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults. N Engl J Med. 2004;351:1741-51.
Thwaites G, Fisher M, Hemingway C, Scott G, Solomon T, Innes J, et al. British infection society guidelines for the diagnosis and treatment of tuberculosis of the central nervous system in adults and children. J infection. 2009;59:167-87.
Dooley DP, Carpenter JL, Rademacher S. Adjunctive corticosteroid therapy for tuberculosis: a critical reappraisal of the literature. Clin Infect Dis 1997;25:872–87.
Trautner BW, Darouiche RO. Tuberculous pericarditis: optimal diagnosis and management. Clin Infect Dis. 2001;33:954-61.
Engel ME, Matchaba PT, Volmink J. Corticosteroids for tuberculous pleurisy. Cochrane Database of Syst Rev. 2007;17:CD001876.
Tongyoo S, Permpikul C, Mongkolpun W, Vattanavanit V, Udompanturak S, Kocak M, et al. Hydrocortisone treatment in early sepsis associated acute respiratory distress syndrome: results of a randomized controlled trial. Critical Care. 2016;20:329.
Meduri GU, Bridges L, Shih MC, Marik PE, Siemieniuk RA, Kocak M. Prolonged glucocorticoid treatment is associated with improved ARDS outcomes: analysis of individual patients’ data from four randomized trials and trial-level meta-analysis of the updated literature. Intensive Care Med. 2016;42:829–40.
World Health Organization. Treatment of tuberculosis: guidelines, 2010.
Chaiprasert A. Future trend in laboratory diagnosis of tuberculosis. Siriraj Med J. 2009;61:45-8.
American Thoracic Society. Diagnostic Standards and Classification of Tuberculosis in Adults and Children. Am J Respir Crit Care Med. 2000;161:1376-95.
Sahn SA, Neff TA. Miliary tuberculosis. Am J Med. 1974;54:495–505.
Therasakvichya S, Choavaratana R, Sompradeekul S. Disseminated tuberculosis. Siriraj Hosp Gaz. 2002;54:484-8.
Bhurayanontachai R, Maneenil K. Factors influencing development and mortality of acute respiratory failure in hospitalized patient with active pulmonary tuberculosis: a 10-year retrospective review. J Thorac Dis. 2016;8:1721-30.
Cheng VC, Ho PL, Lee RA, Chan KS, Chan KK, Woo PC, et al. Clinical spectrum of paradoxical deterioration during antituberculosis therapy in non-HIV-infected patients. Eur J Clin Microbiol Infect Dis. 2002;21:803–9.
Orlovic D, Smego RA. Paradoxical tuberculous reactions in HIV-infected patients. Int J Tuberc Lung Dis. 2001;5:370–5.
Ryu YJ, Koh WJ, Kang EH, Suh GY, Chung MP, Kim H, et al. Prognostic factors in pulmonary tuberculosis requiring mechanical ventilation for acute respiratory failure. Respirology. 2007;12:406-11.
Zahar JR, Azoulay E, Klement E, De Lassence A, Lucet JC, Regnier B, et al. Delayed treatment contributes to mortality in ICU patients with severe active pulmonary tuberculosis and acute respiratory failure. Intensive Care Med. 2001;27:513-20.
Kim YJ, Pack KM, Jeong E, Na JO, Oh YM, Lee SD, et al. Pulmonary tuberculosis with acute respiratory failure. Eur Respir J. 2008;32:1625-30.
Critchly JA, Young F, Orton L, Garner P. Corticosteroids for prevention of mortality in people with tuberculosis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:223-37.
Yang JY, Han M, Koh Y, Kim WS, Song JW, Oh YM, et al. Effects of corticosteroids on critically ill pulmonary tuberculosis patients with acute respiratory failure: a propensity analysis of mortality. CID. 2016;63:1449-55.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




