Burnout syndrome among Thai intensivists and nurses in pre-COVID19 era
Burnout in pre-COVID19
Keywords:
Burnout syndrome, Emotion exhaustion, Depersonalization, Personal accomplishmentAbstract
Background: Burnout syndrome (BOS), a work-related constellation of symptoms and signs, causes individuals emotional stress and is associated with increasing job-related disillusionment. ICU-BOS among Thai intensivists and ICU nurses has never been clarified.
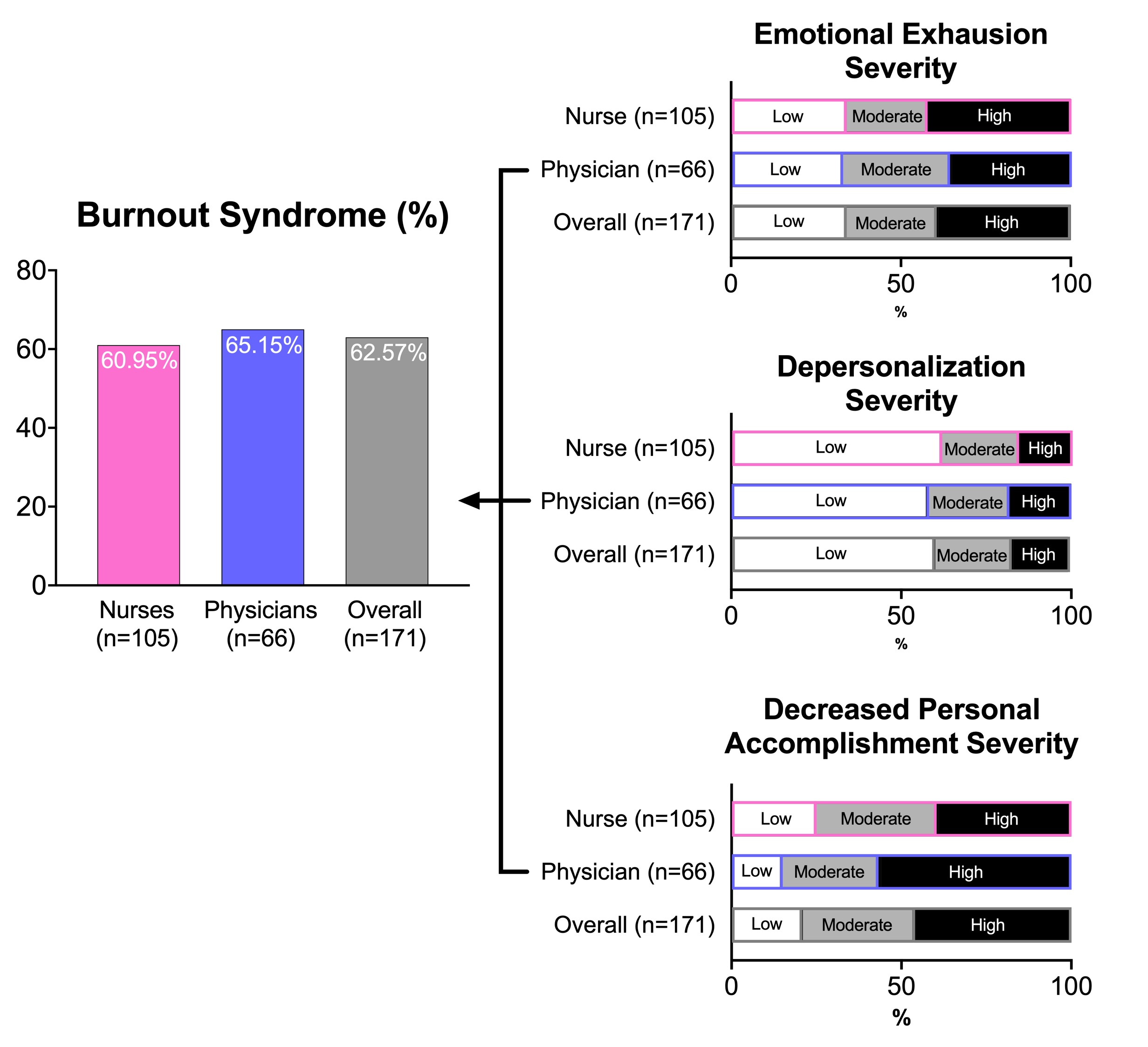
Methods & materials: We performed a multicenter, prospective cross-sectional study in 17 hospitals in Thailand. BOS-related data were collected from full-time ICU physicians and ICU nurses using electronic questionnaires. ICU-BOS was defined when participant exhibited at least 1 of 3 aspects (depersonalization, emotion exhaustion, and personal accomplishment) regarding the Maslach Burnout Inventory. Primary outcome was prevalence of ICU-BOS among intensivists and ICU nurses, and secondary outcomes were risk factors for ICU-BOS.
Results: After a total of 193 electronic surveys were sent, 171 responders (ICU physicians n=66, ICU nurses n=105) were included in this analysis (88.6%). Overall prevalence of ICU-BOS was 62.6%. Using multivariate analysis, the risk factors for ICU-BOS among intensivists were 1) income <20,000 THB, 2) feeling of quitting caring for patients in an ICU within the past 1 year, 3) need >2 holidays/wk. and 4) patient’s ICU-LOS >5 days (adjusted odd ratio (OR) of 31.5, 15.9, 7.4, 14.9; p =0.04, 0.007, 0.035, 0.004 respectively). Risk factors for ICU-BOS among ICU nurses were 1) age >40 years, 2) ICU experience >5 years, 3) patient’s ICU-LOS >5 days, 4) feeling assignments in the ICU were too much and 5) feeling of quitting caring for patients in an ICU within the past 1 year (adjusted OR of 15.7, 4.6, 10.0, 4.3, 5.3; p =0.009, 0.04, 0.004, 0.04, 0.007 respectively).
Conclusions: In this study, we found a high prevalence of ICU-BOS among Thai intensivists and ICU nurses. Co-independent risk factors for BOS were patient’s ICU-LOS >5 days and feeling of quitting caring for patients in an ICU within the past 1 year. Our findings supported further interventions to reduce the high prevalence of ICU-BOS among Thai ICU professionals.
Downloads
References
Kuremyr D, Kihlgren M, Norberg A, Astrom S, Karisson I. Emotional experiences, empathy and burnout among staff caring for demented patients at a collective living unit and a nursing home. J Adv Nurs. 1994; 19:6709.
Youngsri C. Perception of Working Environment, Burnout and Turnover Intentions of Employees. Industrial and Organizational Psychology King Mongkut’s Institute of Technology North Bangkok; 2006.
Lerthattasilp T. Burnout among psychiatrists in Thailand. J Psychiatr Assoc Thailand. 2011; 56(4):437-448.
Sikheawsukwonghot IP. Factors influencing turnover of physicians in Thai public hospitals. Journal of Graduate Study in Humanities and Social Sciences. 2016; 5:183-209.
Shanafelt TD, Sonja B, Litjen T, Dyrbye LN, Sotile W, Daniel S, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. JAMA Intern Med. 2012; 172:1377–85.
Soler JK, Yaman H, Esteva M, Dobbs F, Asenova RS, Katic M, et al. Burnout in European family doctors: the EGPRN study. Fam Pract. 2008; 25:245–65.
Sharma A, Sharp DM, Walker LG, Monson JR. Stress and burnout in colorectal and vascular surgical consultants working in the UK National Health Service. Psychooncology. 2008; 17:570–6.
Maslach C, Leiter MP. The Truth About Burnout. San Francisco, California: Josset-Bass Publishers; 1997.
Sammawart S. Burnout among nurses in Ramathibodi Hospital. (Master of Science thesis) Faculty of Nursing: Mahidol University; 1989. 100p.
Maslach C, Jackson SE. Maslach Burnout Inventory. Manual Research Edition. Palo Alto, California: Consulting Psychologists Press; 1986.
Chien-Huai Chuang MD, Pei-Chi Tseng MD, Chun-Yu Lin PhD, Kuan-Han Lin PhD, Yen-Yuan Chen MD, MPH PhD. Burnout in the intensive care unit professionals A systematic review. Medicine (Baltimore). 2016; 95(50):e5629.
Embriaco N, Papazian L, Kentish-Barnes N, Pochard F, Azoulay E. BOS among critical care healthcare workers. Curr Opin Crit Care. 2007; 13(5):482-488.
Poncet MC, Toullic P, Papazian L. BOS in critical care nursing staff. Am J Respir Crit Care Med. 2007; 175(7):698-704.
Mealer M, Jones J, Newman J, McFann KK, Rothbaum B, Moss M. The presence of resilience is associated with a healthier psychological profile in intensive care unit (ICU) nurses: results of a national survey. Int J Nurs Stud. 2012; 49(3):292-299.