Nocturnal dexmedetomidine for prevention of delirium in critically ill surgical patients: a randomized control trial protocol
Nocturnal dexmedetomidine for delirium prevention in ICU
DOI:
https://doi.org/10.54205/ccc.v30.254777Keywords:
Dexmedetomidine, Surgical intensive care, Postoperative delirium, PreventionAbstract
Background: Nocturnal or postoperative dexmedetomidine has been shown to reduce the incidence of delirium in critically ill surgical patients without an increase in any complications. However, it is not clear whether dexmedetomidine has preventive effect against delirium in the patients with high risk of postoperative delirium (POD) since no previous studies have clearly emphasized high-risk surgical patients.
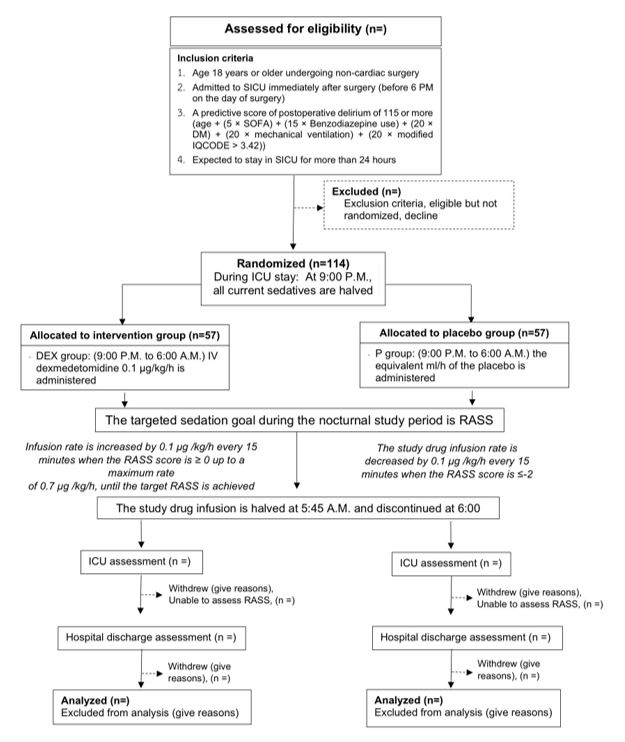
Method: In this single-center, double-blind, randomized controlled trial, we randomize 114 high risk POD patients defined by developed predictive scores and admitted to surgical intensive care units (SICUs) into 2 groups: nocturnal dexmedetomidine (9 pm – 6 am) and placebo. The outcomes were incidence of POD, delirium-free days, secondary delirium-related complications and concerned complications including hypotension and bradycardia. Other treatments apart from intervention are standardized. Intention to treat analysis is used to analyze all data.
Hypothesis: We hypothesize that nocturnal dexmedetomidine giving to high-risk POD patients admitted to SICUs postoperatively would (1) reduce incidence of POD (2) improve delirium-free days (3) reduce secondary delirium-related complications (4) show no difference in hypotension and bradycardia between groups.
Ethics and dissemination: The trial receives ethic approval from Siriraj Institutional Review Board. We plan to disseminate the results in peer-reviewed critical care medicine or anesthesiology-related journals, conferences nationally and internationally.
Trial registration: TCTR20210217001
Downloads
References
Whitlock EL, Vannucci A, Avidan MS. Postoperative delirium. Minerva Anestesiol. 2011;77(4):448–56.
Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJC, Pandharipande PP, et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU: Crit Care Med. 2018;46(9):e825–73.
Gusmao-Flores D, Salluh JIF, Chalhub RÁ, Quarantini LC. The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of delirium: a systematic review and meta-analysis of clinical studies. Crit Care Lond Engl. 2012;16(4):R115.
Janssen TL, Alberts AR, Hooft L, Mattace-Raso F, Mosk CA, van der Laan L. Prevention of postoperative delirium in elderly patients planned for elective surgery: systematic review and meta-analysis. Clin Interv Aging. 2019;14:1095–117.
Moskowitz EE, Overbey DM, Jones TS, Jones EL, Arcomano TR, Moore JT, et al. Post-operative delirium is associated with increased 5-year mortality. Am J Surg. 2017;214(6):1036–8.
Aldecoa C, Bettelli G, Bilotta F, Sanders RD, Audisio R, Borozdina A, et al. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol. 2017;34(4):192–214.
Marcantonio ER. Delirium in Hospitalized Older Adults. Solomon CG, editor. N Engl J Med. 2017;377(15):1456–66.
Chaiwat O, Chanidnuan M, Pancharoen W, Vijitmala K, Danpornprasert P, Toadithep P, et al. Postoperative delirium in critically ill surgical patients: incidence, risk factors, and predictive scores. BMC Anesthesiol. 2019;19(1):39.
Kaur M, Singh P. Current role of dexmedetomidine in clinical anesthesia and intensive care. Anesth Essays Res. 2011;5(2):128.
Su X, Meng Z-T, Wu X-H, Cui F, Li H-L, Wang D-X, et al. Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: a randomised, double-blind, placebo-controlled trial. The Lancet. 2016;388(10054):1893–902.
Skrobik Y, Duprey MS, Hill NS, Devlin JW. Low-Dose Nocturnal Dexmedetomidine Prevents ICU Delirium. A Randomized, Placebo-controlled Trial. Am J Respir Crit Care Med. 2018;197(9):1147–56.
Han JH, Wilson A, Graves AJ, Shintani A, Schnelle JF, Dittus RS, et al. Validation of the Confusion Assessment Method for the Intensive Care Unit in older emergency department patients. Acad Emerg Med Off J Soc Acad Emerg Med. 2014;21(2):180–7.
Pipanmekaporn T, Wongpakaran N, Mueankwan S, Dendumrongkul P, Chittawatanarat K, Khongpheng N, et al. Validity and reliability of the Thai version of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Clin Interv Aging. 2014;9:879–85.
Khan BA, Perkins AJ, Gao S, Hui SL, Campbell NL, Farber MO, et al. The Confusion Assessment Method for the ICU-7 Delirium Severity Scale: A Novel Delirium Severity Instrument for Use in the ICU. Crit Care Med. 2017;45(5):851–7.
Siri S, Okanurak K, Chansirikanjana S, Kitayaporn D, Kitiyaporn D, Jorm AF. Modified Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) as a screening test for dementia for Thai elderly. Southeast Asian J Trop Med Public Health. 2006;37(3):587–94.
Jones AE, Trzeciak S, Kline JA. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit Care Med. 2009;37(5):1649–54.
Wongtangman K, Chaiwat O, Suraseranivongse S, Rn N, Sanansilp V, Wangnamthip S. Validation of the Thai Version Critical Care Pain Observation Tool and Behavioral Pain Scale in Postoperative Mechanically Ventilated ICU Patients. 2017;9–19.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




