The incidence and risk factors of post-extubation dysphagia in critically ill surgical patients: protocol for prospective observational study
DOI:
https://doi.org/10.54205/ccc.v30.254965Keywords:
Dysphagia, Post-extubation dysphagia (PED), Aspiration, Water swallowing test (WST), Fiberoptic endoscopic evaluation of swallowing (FEES)Abstract
Background: Post-extubation dysphagia (PED) is commonly reported in critically ill patients. Although dysphagia is not a fatal disease, it is an important medical condition that required the appropriate treatment. Early detection of PED is essential to reduce complications. There is no well-established standard screening and treatment protocol for surgical intensive care unit. The aims of this study are to report the incidence and identify the risk factors of PED in critically ill surgical patients.
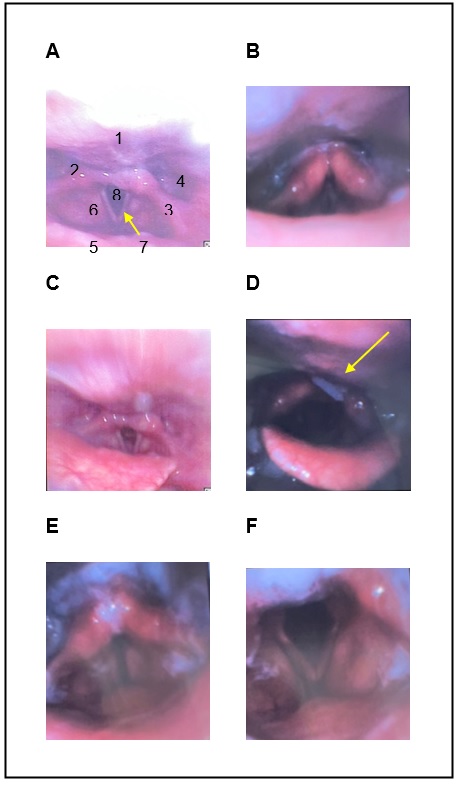
Methods: This study is a prospective observational study. Two hundred patients who are intubated and on mechanical ventilation for ≥ 24 hours and successfully extubated without exclusion are needed to be enrolled. The patients will be performed water swallowing test (WST) at bedside in surgical ICU within 3-6 hours after extubation. For those patients who failed the WST, swallowing specialists will perform bedside fiberoptic endoscopic evaluation of swallowing (FEES) in SICU within 24-48 hours to establish the diagnosis of dysphagia. The primary outcome is the incidence and risk factors of post-extubation dysphagia. The secondary outcomes include time to resume oral diet after extubation, Functional Oral Intake Scale at follow-up, and adverse outcomes related with PED.
Discussion: The early detection of PED could be accomplished by using an effective screening tool, the WST, and confirmed the diagnosis by FEES performed by swallowing specialists. The incidence and risk factors of PED reported in this study will be helpful in developing the protocol for screening and treatment for PED in critically ill surgical patients.
Trial registration: The Thai Clinical Trials Registry (TCTR20211023003)
Registered on 23 October 2021
Downloads
References
Schefold JC, Berger D, Zürcher P, Lensch M, Perren A, Jakob SM, et al. Dysphagia in Mechanically Ventilated ICU Patients (DYnAMICS): A Prospective Observational Trial. Crit Care Med. 2017;45:2061-9.
Skoretz SA, Flowers HL, Martino R. The incidence of dysphagia following endotracheal intubation: a systematic review. Chest. 2010;137:665-73.
McIntyre M, Doeltgen S, Dalton N, Koppa M, Chimunda T. Post-extubation dysphagia incidence in critically ill patients: A systematic review and meta-analysis. Aust Crit Care. 2021;34:67-75.
El Gharib AZG, Berretin-Felix G, Rossoni DF, Seiji Yamada S. Effectiveness of Therapy on Post-Extubation Dysphagia: Clinical and Electromyographic Findings. Clin Med Insights Ear Nose Throat. 2019;12:1179550619873364.
Macht M, Wimbish T, Bodine C, Moss M. ICU-acquired swallowing disorders. Crit Care Med. 2013;41:2396-405.
Zuercher P, Schenk NV, Moret C, Berger D, Abegglen R, Schefold JC. Risk Factors for Dysphagia in ICU Patients After Invasive Mechanical Ventilation. Chest. 2020;158:1983-91.
Brodsky MB, Pandian V, Needham DM. Post-extubation dysphagia: a problem needing multidisciplinary efforts. Intensive Care Med. 2020;46:93-6.
Christensen M, Trapl M. Development of a modified swallowing screening tool to manage post-extubation dysphagia. Nurs Crit Care. 2018;23:102-7.
Johnson KL, Speirs L, Mitchell A, Przybyl H, Anderson D, Manos B, et al. Validation of a Postextubation Dysphagia Screening Tool for Patients After Prolonged Endotracheal Intubation. Am J Crit Care. 2018;27:89-96.
Moraes DP, Sassi FC, Mangilli LD, Zilberstein B, de Andrade CR. Clinical prognostic indicators of dysphagia following prolonged orotracheal intubation in ICU patients. Crit Care. 2013;17:R243.
Perren A, Zürcher P, Schefold JC. Clinical Approaches to Assess Post-extubation Dysphagia (PED) in the Critically Ill. Dysphagia. 2019;34:475-86.
Wu CP, Xu YJ, Wang TG, Ku SC, Chan DC, Lee JJ, et al. Effects of a swallowing and oral care intervention for patients following endotracheal extubation: a pre- and post-intervention study. Crit Care. 2019;23:350.
Brodsky MB, Mayfield EB, Gross RD. Clinical Decision Making in the ICU: Dysphagia Screening, Assessment, and Treatment. Semin Speech Lang. 2019;40:170-87.
Regala M, Marvin S, Ehlenbach WJ. Association Between Postextubation Dysphagia and Long-Term Mortality Among Critically Ill Older Adults. J Am Geriatr Soc. 2019;67:1895-901.
Brodsky MB, Suiter DM, González-Fernández M, Michtalik HJ, Frymark TB, Venediktov R, et al. Screening Accuracy for Aspiration Using Bedside Water Swallow Tests: A Systematic Review and Meta-Analysis. Chest. 2016;150:148-63.
Leder SB, Warner HL, Suiter DM, Young NO, Bhattacharya B, Siner JM, et al. Evaluation of Swallow Function Post-Extubation: Is It Necessary to Wait 24 Hours? Ann Otol Rhinol Laryngol. 2019;128:619-24.
Sassi FC, Medeiros GC, Zilberstein B, Jayanthi SK, de Andrade CRF. Screening protocol for dysphagia in adults: comparison with videofluoroscopic findings. Clinics (Sao Paulo). 2017;72:718-22.
Siriraj. Swollowing screening sheet. Edited by sheet Ss: 2020.
Borders JC, Brates D. Use of the Penetration-Aspiration Scale in Dysphagia Research: A Systematic Review. Dysphagia. 2020;35:583-97.
Scheel R, Pisegna JM, McNally E, Noordzij JP, Langmore SE. Endoscopic Assessment of Swallowing After Prolonged Intubation in the ICU Setting. Ann Otol Rhinol Laryngol. 2016;125:43-52.
Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86:1516-20.
McMicken BL, Muzzy CL, Calahan S. Retrospective ratings of 100 first time-documented stroke patients on the Functional Oral Intake Scale. Disabil Rehabil. 2010;32:1163-72.
Dennis MS, Lewis SC, Warlow C. Effect of timing and method of enteral tube feeding for dysphagic stroke patients (FOOD): a multicentre randomised controlled trial. Lancet. 2005;365:764-72.
Jongprasitkul H, Kitisomprayoonkul W. Effectiveness of Conventional Swallowing Therapy in Acute Stroke Patients with Dysphagia. Rehabil Res Pract. 2020;2020:2907293.
Foley N, Teasell R, Salter K, Kruger E, Martino R. Dysphagia treatment post stroke: a systematic review of randomised controlled trials. Age Ageing. 2008;37:258-64.
Zuercher P, Moret CS, Dziewas R, Schefold JC. Dysphagia in the intensive care unit: epidemiology, mechanisms, and clinical management. Crit Care. 2019;23:103.
Suiter DM, Sloggy J, Leder SB. Validation of the Yale Swallow Protocol: a prospective double-blinded videofluoroscopic study. Dysphagia. 2014;29:199-203.
Rassameehiran S, Klomjit S, Mankongpaisarnrung C, Rakvit A. Postextubation Dysphagia. Proc (Bayl Univ Med Cent). 2015;28:18-20.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




