Effect of milrinone versus placebo on hemodynamic in patients with septic shock: A randomize control trial
DOI:
https://doi.org/10.54205/ccc.v30.255002Keywords:
Milrinone, Septic shock, Cardiac output, Poor tissue perfusionAbstract
Background: Sepsis is one of the most serious healthcare problems worldwide, which is associated with high mortality and financial burdens. The common causes of death are refractory shock and multi-organ failure. Myocardial dysfunction, a relatively common complication of septic shock, causes a significantly decrease in stroke volume and cardiac output. This results in insufficient blood supply to the organs, creates multi-organ failure and finally, leading to death. The Surviving Sepsis Campaign Guidelines 2016 also recommended using dobutamine in septic shock patients who had been resuscitated until achieving normal blood pressure target of mean arterial pressure 65 mmHg or more, but still had evidence of inadequate tissue perfusion. Milrinone action via an alternative pathway from the sympathetic inotropic agents, makes the milrinone to be used as an option for improve cardiac function among sepsis patients. However, there are few studies of milrinone in patients with
septic shock.
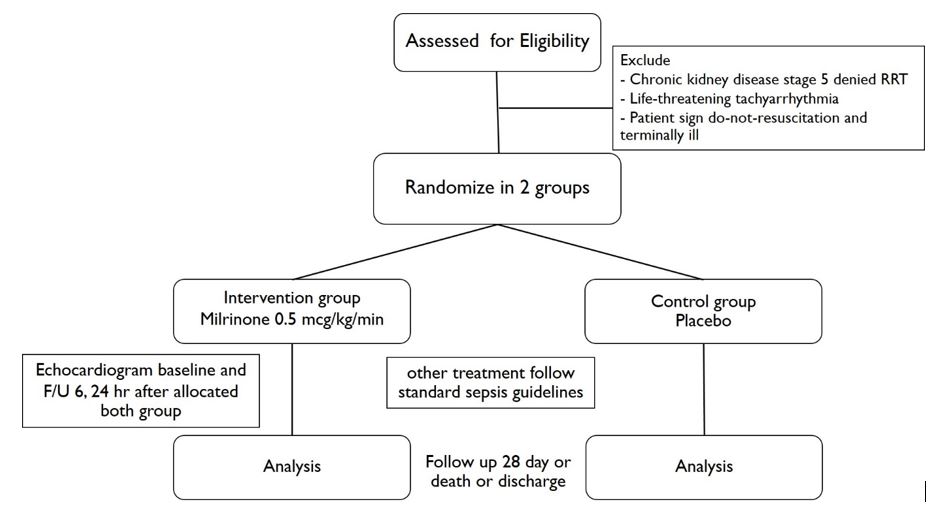
Methods: We plan to conduct a double blind randomized controlled trial, enrolling patients at Siriraj hospital and Hat-Yai hospital. The adults with the diagnosis of septic shock according to definition of SEPSIS III will be screened. Patients who receive fluid resuscitation at least 30 mL/kg, mean arterial pressure (MAP) ≥ 65 mmHg, with a clinical sign of poor tissue perfusion, or evidence of impaired left ventricular systolic function (left ventricular ejection fraction (LVEF) < 40%) will be enrolled. The patients were randomly assigned in a 1:1 ratio by their sequential number to receive either milrinone (intervention group) or placebo (control group). The physician performs an echocardiogram for assessing cardiac function, before the starting of the study drug and after the 6 and 24 hours. The monitoring of vital signs, urine output, and lactate at 6 and 24 hours after milrinone or placebo commencement is recorded.
Conclusion: This study will evaluate the efficacy of milrinone in improving cardiac output among adult patients with septic shock who is resuscitated to achieve target blood pressure but still have signs of poor tissue perfusion.
Downloads
References
Fleischmann C, Scherag A, Adhikari NK, et al. Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations. Am J Respir Crit Care Med. 2016; 193(3): 259-72.
Phua J, Koh Y, Du B, Tang YQ, Jigeeshu V, Divatia JV, et al. Management of severe sepsis in patients admitted to Asian intensive care units: prospective cohort study. BMJ. 2011;342:d3245.
Angkasekwinai N, Rattanaumoawan P, Thamlikitkul V. Epidemiology of sepsis in Siriraj Hospital 2007. J Med Assoc Thai. 2009, 2:S68-78
Moskowitz A, Omar Y, Chase M, Lokhandwala S, Patel P, Abdersen LW, et al. Reasons for Death in Patients with Sepsis and Septic Shock. J Crit Care. 2017; 38: 284–8
Vincent JL, Nelson DR, Williams MD. Is worsening multiple organ failure the cause of death in patients with severe sepsis?. Crit Care Med. 2011;39:1050-5
Sato R, Kuriyama A, Takada T, Nasu M, Luthe SK. Prevalence and risk factors of sepsis-induced cardiomyopathy: a retrospective cohort study. Medicine. 2016;95(39):e5031.
Tongyoo S, Permpikul C, Lertsawangwong S et al. Right ventricular dysfunction in septic shock: a retrospective cohort study J Med Assoc Thai. 2011; 94: S188-S195
Chayakul W, Tongyoo S, Permpikul C. Incidence and Outcomes of Sepsis-Related Cardiomyopathy: A Prospective Cohort Study. J Med Assoc Thai 2021;104:497-505
Song MJ, Lee SH, Leem AY, et al. Predictors and outcomes of sepsis-induced cardiomyopathy in critically ill patients. Acute Crit Care. 2020;35(2):67–76
Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368-1377.
Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43(3):304-377
Hernandez G, Bruhn A, Luengo C, et al. Effects of dobutamine on systemic, regional and microcirculatory perfusion parameters in septic shock: a randomized, placebo-controlled, double-blind, crossover study. Intensive Care Med. 2013;39(8):1435-43.
Kumar A, Schupp E, Bunnell E, et al. Cardiovascular response to dobutamine stress predicts outcome in severe sepsis and septic shock. Crit Care. 2008;12(2):R35.
Sato R, Ariyoshi N, Hasegawa D, et al. Effects of Inotropes on the Mortality in Patients with Septic Shock. J Intensive Care Med 2019; 885066619892218
Barton P, Garcia J, Kouatli A, et al: Hemodynamic effects of i.v. milrinone lactate in pediatric patients with septic shock. A prospective, double-blinded, randomized, placebo-controlled, interventional study. Chest. 1996; 109:1302–1312
Wang Z, Wu Q, Nie X, et al. Combination therapy with milrinone and esmolol for heart protection in patients with severe sepsis: a prospective, randomized trial. Clin Drug Investig. 2015;35(11):707-16.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




