Respiratory variation of central vein diameter in upper body as a surrogate of pulse pressure variation
DOI:
https://doi.org/10.54205/ccc.v30.255038Keywords:
Pulse pressure variation, Internal jugular vein, Subclavian vein, Brachiocephalic vein, Variability index, Distensibility index, Collapsibility index, Respiratory variationAbstract
Background: Cyclical change in central vein diameter during respiratory cycle can be used for fluid-responsiveness assessment. The purpose of this study is to assess variations in the diameter of central veins in upper body region, specifically internal jugular vein (IJV), subclavian vein (SCV), and brachiocephalic vein (BCV), in mechanically ventilated patients. We hypothesized that variations in the diameter of these veins caused by passive ventilation would be strongly concordant with pulse pressure variation (PPV).
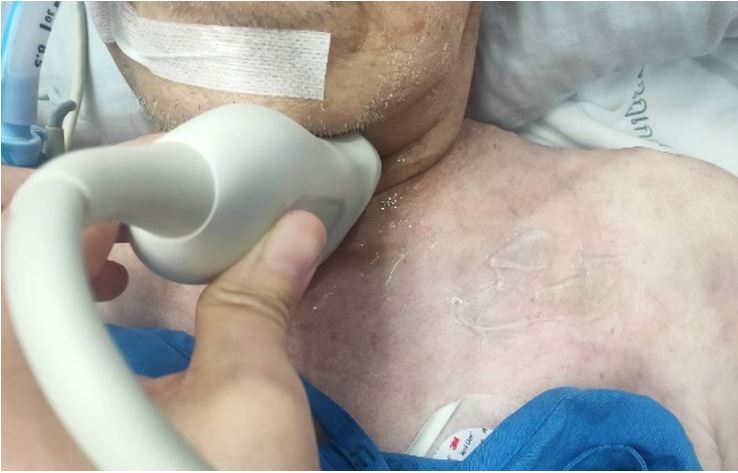
Methods: The study was conducted in mechanically ventilated, critically ill surgical and medical patients. The PPV values were automatically calculated and were recorded. The diameters of the study veins such as the IJV, SCV, and BCV were measured bedside using the ultrasound. Then respiratory variations of venous diameter were calculated into distensibility index, collapsibility index and variability index. The relationships between PPV and ultrasound-derived parameters were assessed. Patients were separated into two groups according to their PPV values (>13 and <10). The test performance and proper cut-off values of ultrasound-derived parameters to distinguish between these two groups were generated by receiver operating characteristic (ROC) curves.
Results: A total of 44 patients were assessed. There were substantial correlations between PPV and ultrasound parameter namely IJV-DI (r=0.652, p<0.001), IJV-VI (r=0.655, p<0.001), SCV-CI (r=0.618, p<0.001), and SCV-VI (r=0.626, p<0.001). While PPV and BCV-CI show moderate correlation (r=0.531, p=0.008). The IJV-DI, IJV-VI, SCV-CI, SCV-VI and BCV-VI values were significantly greater in PPV>13 group than PPV<10 group. All these parameters were effective in distinguishing between PPV>13 from PPV<10 group with AUC 0.983, 0.983, 0.928, 0.928 and 0.826, respectively. The IJV-DI, IJV-VI, SCV-CI, SCV-VI and BCV-VI analysis demonstrated appropriate cut-off values for separating patients with PPV>13 from those with PPV<10 as 16.19% (sensitivity 92%, specificity 96%), 14.98 % (sensitivity 92%, specificity 96%), 9.74% (sensitivity of 93%, specificity of 91%), 12.33% (sensitivity of 87%, specificity of 100%) and 13.71% (sensitivity of 73%, specificity of 100%), respectively.
Conclusions: In critically ill patients, all ultrasound-derived measures such as IJV-DI, IJV-VI, SCV-CI, SCV-VI, and BCV-VI revealed significant correlation with PPV value.
Downloads
References
Granado RC, Mehta RL. Fluid overload in the ICU: evaluation and management. BMC Nephrol. 2016; 17:109
Monnet X, Marik PE, Teboul JL. Prediction of fluid responsiveness: an update. Ann Intensive Care. 2016; 6:111
Vignon P, Repessé X, Bégot E, Léger J, Jacob C, Bouferrache K, et al. Comparison of Echocardiographic Indices Used to Predict Fluid Responsiveness in Ventilated Patients. Am J Respir Crit Care Med. 2017; 195(8):1022-1032
Hasanin A, Mostafa M. Evaluation of fluid responsiveness during COVID-19 pandemic: what are the remaining choices? J Anesth. 2020; 34:758-64
Giraud R, Abraham PS, Brindel P, Siegenthaler N, Bendjelid K. Respiratory changes in subclavian vein diameters predicts fluid responsiveness in intensive care patients: a pilot study. J Clin Monit Comput. 2018; 32:1049-55
Yang X, Du B. Does pulse pressure variation predict fluid responsiveness in critically ill patients? A systematic review and meta-analysis. Critical Care. 2014; 18:650
Marik PE, Cavallazzi R, Vasu T, Hirani A. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med. 2009; 37: 2642-7
Guarracino F, Ferro B, Forfori F, Bertini P, Magliacano L, Pinsky MR. Jugular vein distensibility predicts fluid responsiveness in septic patients. Critical Care. 2014; 18:647
Jouffroy R, Liaudet BP, Neel V, Vivien B. Interchangeability between respiratory variation of subclavian vein and pulse pressure variation in ventilated patients in the operating room. Turk J Anaesthesiol Reanim. 2020; 48(6): 467-72
Miller A, Mandeville J. Predicting and measuring fluid responsiveness with echocardiography. Echo Res Pract. 2016; 3(2): G1-G12
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




