Comparison of ultrasound assessment for diaphragmatic workload during spontaneous breathing trial between automatic tube compensation and pressure support ventilation: Study protocol
DOI:
https://doi.org/10.54205/ccc.v30.255057Keywords:
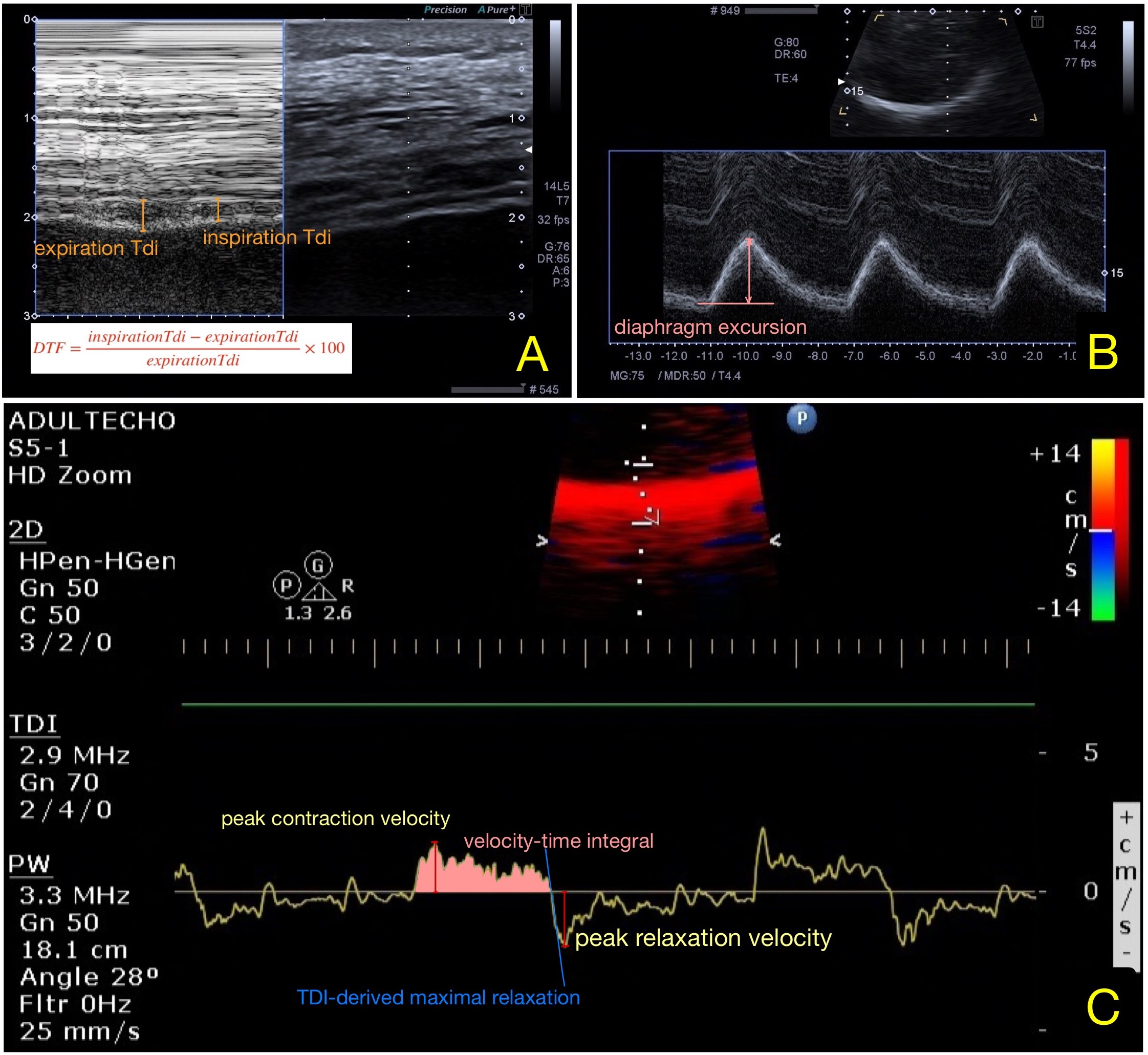
Automatic tube compensation, Pressure support ventilation, Ultrasound diaphragm, Diaphragm thickness fraction, TDI-derived maximal relaxation rateAbstract
Background: The process of weaning from mechanical ventilation is crucial. Less demanding spontaneous breathing trials (SBT) can be done by either automatic tube compensation (ATC) or pressure support ventilation (PSV) to decrease inspiratory effort by endotracheal tube resistance compensation. This study aimed to assess the patient’s effort, by diaphragm ultrasonography with ATC compared to PSV during SBT.
Methods: Patients who have been on mechanical ventilation for more than 48 hours and meet the weaning requirements are given 30 minutes for ATC and 30 minutes for PSV in this randomized control experiment. The diaphragm workload difference, as assessed by diaphragm thickness fraction, was the primary outcome. The sensitivity and specificity of ultrasound-measured diaphragmatic muscle activity measures in predicting ventilator weaning and effective extubation were secondary outcomes.
Hypothesis: Intubated patients should be (1) weaning with lower effort SBT mode (2) predicted weaning success with more accurately parameters
Ethics and dissemination: Ramathibodi Human Research Ethics Committee has approved the trial. The findings plan to summitted in peer-reviewed publications and conferences in critical care medicine or anesthesiology.
Trial registration number: TCTR20210317004
Downloads
References
Burns SM. Making Weaning Easier. Crit Care Nurs Clin North Am. 1999;11(4):465–77.
Epstein CD, El-Mokadem N, Peerless JR. Weaning older patients from long-term mechanical ventilation: a pilot study. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses. 2002;11(4):369–77.
Torres A, Gatell JM, Aznar E, el-Ebiary M, Puig de la Bellacasa J, González J, et al. Re-intubation increases the risk of nosocomial pneumonia in patients needing mechanical ventilation. Am J Respir Crit Care Med. 1995;152(1):137–41.
Marino PL. Marino’s the ICU book. 4th ed. USA: Lippincott Williams & Wilkins; 2014.
Boles J-M, Bion J, Connors A, Herridge M, Marsh B, Melot C, et al. Weaning from mechanical ventilation. Eur Respir J. 2007; 29(5):1033–56.
Subirà C, Hernández G, Vázquez A, Rodríguez-García R, González-Castro A, García C, et al. Effect of Pressure Support vs T-Piece Ventilation Strategies During Spontaneous Breathing Trials on Successful Extubation Among Patients Receiving Mechanical Ventilation: A Randomized Clinical Trial. JAMA. 2019; 321(22):2175–82.
Guttmann J, Haberthür C, Mols G, Lichtwarck-Aschoff M. Automatic tube compensation (ATC). Minerva Anestesiol. 2002; 68(5):369–77.
Selek Ç, Özcan PE, Orhun G, Şentürk E, Akıncı İÖ, Çakar N. The Comparison of Automatic Tube Compensation (ATC) and T-piece During Weaning. Turk J Anaesthesiol Reanim. 2014; 42(2):91–5.
Cohen J, Shapiro M, Grozovski E, Fox B, Lev S, Singer P. Prediction of extubation outcome: a randomised, controlled trial with automatic tube compensation vs. pressure support ventilation. Crit Care Lond Engl. 2009; 13(1):R21.
Bien M-Y, Shui Lin Y, Shih C-H, Yang Y-L, Lin H-W, Bai K-J, et al. Comparisons of predictive performance of breathing pattern variability measured during T-piece, automatic tube compensation, and pressure support ventilation for weaning intensive care unit patients from mechanical ventilation. Crit Care Med. 2011; 39(10):2253–62.
El-Beleidy ASE-D, Khattab AAE-H, El-Sherbini SA, Al-Gebaly HF. Automatic Tube Compensation versus Pressure Support Ventilation and Extubation Outcome in Children: A Randomized Controlled Study. ISRN Pediatr. 2013; 2013:871376.
Guérin C, Terzi N, Mezidi M, Baboi L, Chebib N, Yonis H, et al. Low-pressure support vs automatic tube compensation during spontaneous breathing trial for weaning. Ann Intensive Care. 2019; 9(1):137.
Tobin MJ. Extubation and the myth of “minimal ventilator settings.” Am J Respir Crit Care Med. 2012; 185(4):349–50.
Llamas-Álvarez AM, Tenza-Lozano EM, Latour-Pérez J. Diaphragm and Lung Ultrasound to Predict Weaning Outcome: Systematic Review and Meta-Analysis. Chest. 2017; 152(6):1140–50.
Vivier E, Muller M, Putegnat J-B, Steyer J, Barrau S, Boissier F, et al. Inability of Diaphragm Ultrasound to Predict Extubation Failure: A Multicenter Study. Chest. 2019; 155(6):1131–9.
Soilemezi E, Savvidou S, Sotiriou P, Smyrniotis D, Tsagourias M, Matamis D. Tissue Doppler Imaging of the Diaphragm in Healthy Subjects and Critically Ill Patients. Am J Respir Crit Care Med. 2020; 202(7):1005–12.
Zein H, Baratloo A, Negida A, Safari S. Ventilator Weaning and Spontaneous Breathing Trials; an Educational Review. Emerg Tehran Iran. 2016; 4(2):65–71.
Umbrello M, Formenti P, Longhi D, Galimberti A, Piva I, Pezzi A, et al. Diaphragm ultrasound as indicator of respiratory effort in critically ill patients undergoing assisted mechanical ventilation: a pilot clinical study. Crit Care Lond Engl. 2015; 19:161.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




