High-protein delivery in mechanically ventilated patients: A study protocol for a randomized trial
High protein delivery in critically ill patients
DOI:
https://doi.org/10.54205/ccc.v31.255072Keywords:
Critically ill, Intensive care units, Mechanically ventilated patients, Nutrition, High proteinAbstract
Background: Critically ill patients are at risk of malnutrition; thus, optimal nutrition delivery is a key treatment for better outcomes. Inadequate energy and protein intake increase rate of hospital-acquired infection, duration of mechanical ventilation and mortality. However, there is no clear consensus regarding optimal protein dose in mechanically ventilated patients. In this study, we aim to compare between the effect of high and usual protein delivery on clinical outcomes in this patient group.
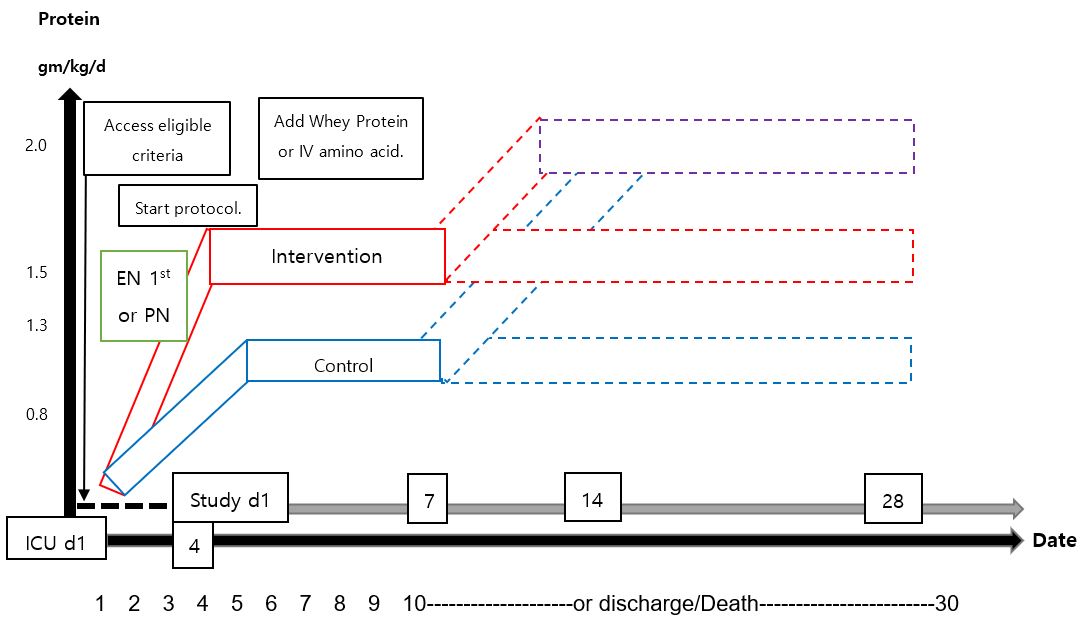
Methods: This is a single-centered, open-labelled, parallel-group, randomized controlled study conducting in medical, surgical and trauma intensive care units (ICU) at a tertiary university hospital in Bangkok, Thailand. We plan to enroll 240 adult mechanically ventilated patients who are expected to require ventilator support for at least 3 days. The intervention group will be prescribed high protein dose (at least 1.5 g/kg/day) throughout ICU stay since day 4 until a maximum of 28 days, whereas the control group will be prescribed usual protein dose (1-1.3 g/kg/day). Nutrition is provided by enteral or parenteral route or both. The primary outcome is ventilator-free days at 28 days. The main secondary outcomes include the temporal change in muscle mass and SOFA score, rate of nosocomial infection and 28-day mortality.
Conclusion: The robust evidence whether delivering high protein in critically ill patients improves outcome is lacking. This randomized trial will examine the consequence of high protein delivery in ICU population.
Downloads
References
Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019;38(1):48-79.
Singer P. Preserving the quality of life: nutrition in the ICU. Crit Care 2019;23(Suppl 1):139.
Elke G, Wang M, Weiler N, Day AG, Heyland DK. Close to recommended caloric and protein intake by enteral nutrition is associated with better clinical outcome of critically ill septic patients: secondary analysis of a large international nutrition database. Crit Care 2014;18(1):R29.
Fetterplace K, Beach LJ, MacIsaac C, Presneill J, Edbrooke L, Parry SM, et al. Associations between nutritional energy delivery, bioimpedance spectroscopy and functional outcomes in survivors of critical illness. J Hum Nutr Diet 2019;32(6):702-12.
Villet S, Chiolero RL, Bollmann MD, Revelly JP, Cayeux RNM, Delarue J, et al. Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr 2005;24(4):502-9.
Weijs PJ, Stapel SN, de Groot SD, Driessen RH, de Jong E, Girbes AR, et al. Optimal protein and energy nutrition decreases mortality in mechanically ventilated, critically ill patients: a prospective observational cohort study. JPEN J Parenter Enteral Nutr 2012;36(1):60-8.
Lew CCH, Wong GJY, Cheung KP, Fraser RJL, Chua AP, Chong MFF, et al. The association between nutritional adequacy and 28-day mortality in the critically ill is not modified by their baseline nutritional status and disease severity. Crit Care 2019;23(1):222.
Looijaard W, Dekker IM, Beishuizen A, Girbes ARJ, Oudemans-van Straaten HM, Weijs PJM. Early high protein intake and mortality in critically ill ICU patients with low skeletal muscle area and -density. Clin Nutr 2020;39(7):2192-201.
Elke G, Wang M, Weiler N, Day AG, Heyland DK. Close to recommended caloric and protein intake by enteral nutrition is associated with better clinical outcome of critically ill septic patients: secondary analysis of a large international nutrition database. Crit Care 2014;18(1):R29.
Zusman O, Theilla M, Cohen J, Kagan I, Bendavid I, Singer P. Resting energy expenditure, calorie and protein consumption in critically ill patients: a retrospective cohort study. Crit Care 2016;20(1):367.
Allingstrup MJ, Kondrup J, Wiis J, Claudius C, Pedersen UG, Hein-Rasmussen R, et al. Early goal-directed nutrition versus standard of care in adult intensive care patients: the single-centre, randomised, outcome assessor-blinded EAT-ICU trial. Intensive Care Med 2017;43(11):1637-47.
Chapple LS, Summers MJ, Bellomo R, Chapman MJ, Davies AR, Ferrie S, et al.; TARGET investigator collaborative and the ANZICS clinical trials group. Use of a high-protein enteral nutrition formula to increase protein delivery to critically ill patients: A randomized, blinded, parallel-group, feasibility trial. JPEN J Parenter Enteral Nutr 2021;45(4):699-709.
Nakamura K, Nakano H, Naraba H, Mochizuki M, Takahashi Y, Sonoo T, et al. High protein versus medium protein delivery under equal total energy delivery in critical care: A randomized controlled trial. Clin Nutr 2021;40(3):796-803.
Doig GS, Simpson F, Bellomo R, Heighes PT, Sweetman EA, Chesher D, et al. Intravenous amino acid therapy for kidney function in critically ill patients: a randomized controlled trial. Intensive Care Med 2015;41(7):1197-208.
Hoffer LJ, Bistrian BR. Appropriate protein provision in critical illness: a systematic and narrative review. Am J Clin Nutr 2012;96(3):591-600.
Berger MM, Reintam-Blaser A, Calder PC, Casaer M, Hiesmayr MJ, Mayer K, et al. Monitoring nutrition in the ICU. Clin Nutr 2019;38(2):584-593.
Compher C, Bingham AL, McCall M, Patel J, Rice TW, Braunschweig C, et al. The american society for parenteral and enteral nutrition. JPEN J Parenter Enteral Nutr 2022;46(1):12-41.
Tongyoo S, Permpikul C, Mongkolpun W, Vattanavanit V, Udompanturak S, Kocak M, et al. Hydrocortisone treatment in early sepsis-associated acute respiratory distress syndrome: results of a randomized controlled trial. Crit Care 2016;20(1):329.
Yehya N, Harhay MO, Curley MAQ, Schoenfeld DA, Reeder RW. Reappraisal of ventilator-free days in critical care research. Am J Respir Crit Care Med 2019;200(7):828-836.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




