Evaluation of weaning parameters for weaning readiness from mechanical ventilation among elderly patients
DOI:
https://doi.org/10.54205/ccc.v30.259010Keywords:
Weaning readiness, Weaning parameters, Mechanical ventilator, Elderly patientsAbstract
Background: Numbers of elderly patients with acute respiratory failure continue to rise with increasing age of the general population worldwide. Ventilatory reserve decreases substantially with age as a result of multiple interrelated physiologic changes.
Objective: This study aimed to evaluate the predictive value of conventional and composite weaning parameters among elderly patients.
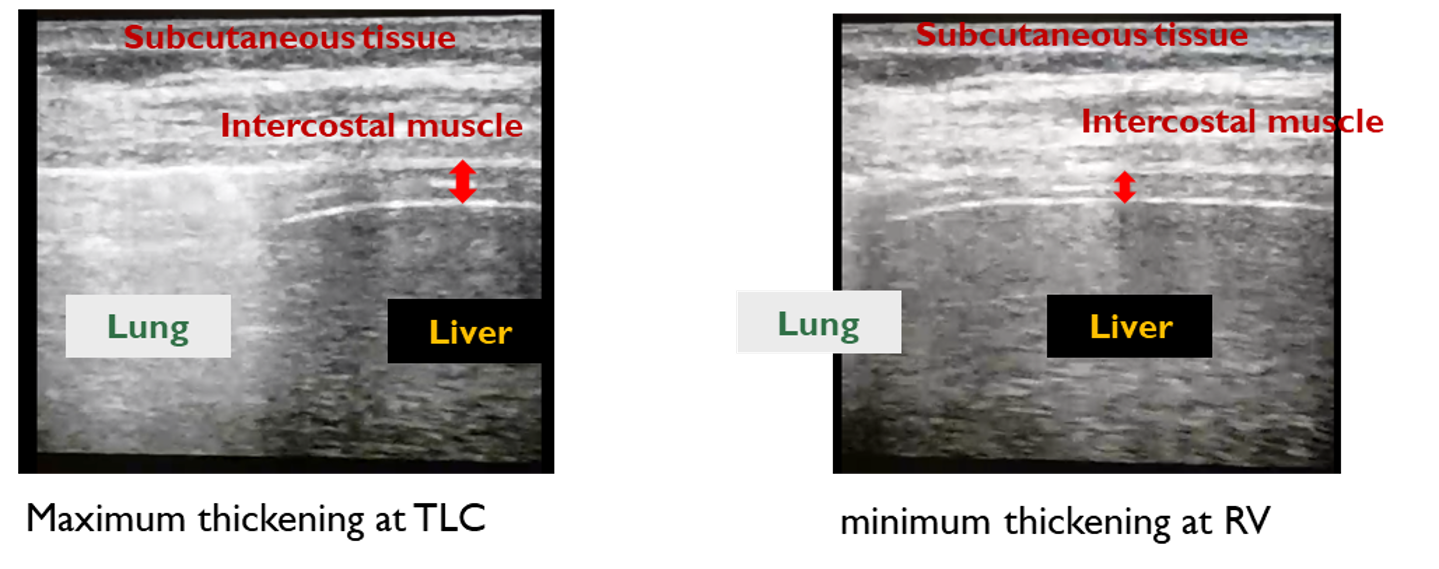
Methods: We conducted an observational prospective study among intubated patients ≥70 years old and readied for undergoing spontaneous breathing trial (SBT). Weaning parameters were recorded [heart rate, respiratory rate, tidal volume, minute ventilation (MV)] at 1 min, 30 min, and 2 hr after beginning of SBT. Cough peak expiratory flow (CPEF) and diaphragmatic thickness (DT) were also measured at 1 min after SBT. Weaning parameters were compared between the 2 patient groups (weaning success vs. weaning failure). Primary outcome was difference in weaning parameters between the 2 groups of patients.
Results: All 48 subjects were enrolled. The mean (±SD) age was 80.2 (±6) years. Altogether, 38 patients (79.2%) were in the weaning success group and 10 patients (20.8%) in the weaning failure group. All baseline characteristics did not significantly differ between the 2 groups. While no difference was observed in other isolated weaning parameters between the 2 patient groups, we found that patients in the weaning success group had significantly lower MV than patients in the weaning failure group (8.3±1.8 vs. 9.9±2.5 L/min, p=0.025). Composite weaning parameters included MV/CPEF and MV/(CPEF x DT) increased predictive values for weaning failure than isolated MV with area under the receiver operating characteristics curves of 0.78, 0.80, and 0.72 respectively. The best cutoff point to predict weaning failure were MV ≥8.4 L/min, MV/CPEF ≥0.12, and MV/(CPEF x DT) ≥0.45 cm-1
Conclusion: MV was the only parameter associated with weaning failure among the elderly. Composite parameters demonstrated better predictive value for assessing weaning readiness among elderly patients.
Downloads
References
Roch A, Wiramus S, Pauly V, Forel JM, Guervilly C, Gainnier M, et al. Long-term outcome in medical patients aged 80 or over following admission to an intensive care unit. Crit Care 2011;15:R36.
Delerme S, Ray P. Acute respiratory failure in the elderly: diagnosis and prognosis. Age Ageing 2008;37:251-7.
Azevedo LC, Park M, Salluh JI, Rea-Neto A, Souza-Dantas VC, Varaschin P, et al. Clinical outcomes of patients requiring ventilatory support in Brazilian intensive care units: a multicenter, prospective, cohort study. Crit Care 2013;17:R63.
Kao KC, Hsieh MJ, Lin SW, Chuang LP, Chang CH, Hu HC, et al. Survival predictors in elderly patients with acute respiratory distress syndrome: a prospective observational cohort study. Sci Rep 2018;8:13459.
Azeredo LM, Nemer SN, Barbas CS, Caldeira JB, Noé R, Guimarães BL, et al. The Integrative Weaning Index in Elderly ICU Subjects. Respir Care 2017;62:333-9.
Fujii M, Iwakami S, Takagi H, Itoigawa Y, Ichikawa M, Iwakami N, et al. Factors influencing weaning from mechanical ventilation in elderly patients with severe pneumonia. Geriatr Gerontol Int 2012;12:277-83.
El Solh AA, Bhat A, Gunen H, Berbary E. Extubation failure in the elderly. Respir Med 2004;98:661-8.
Su KC, Tsai CC, Chou KT, Lu CC, Liu YY, Chen CS, et al. Spontaneous breathing trial needs to be prolonged in critically ill and older patients requiring mechanical ventilation. J Crit Care 2012;27:324.e1-7.
Gao F, Yang LH, He HR, Ma XC, Lu J, Zhai YJ, et al. The effect of reintubation on ventilator-associated pneumonia and mortality among mechanically ventilated patients with intubation: A systematic review and meta-analysis. Heart Lung 2016;45:363-71.
Sharma G, Goodwin J. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging 2006;1:253-60.
Suraseranivong R, Krairit O, Theerawit P, Sutherasan Y. Association between age-related factors and extubation failure in elderly patients. PLoS One 2018;13:e0207628.
Krieger BP, Isber J, Breitenbucher A, Throop G, Ershowsky P. Serial measurements of the rapid-shallow-breathing index as a predictor of weaning outcome in elderly medical patients. Chest 1997;112:1029-34.
Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991;324:1445-50.
Umbrello M, Formenti P, Longhi D, Galimberti A, Piva I, Pezzi A, et al. Diaphragm ultrasound as indicator of respiratory effort in critically ill patients undergoing assisted mechanical ventilation: a pilot clinical study. Crit Care 2015;19:161.
Farghaly S, Hasan AA. Diaphragm ultrasound as a new method to predict extubation outcome in mechanically ventilated patients. Aust Crit Care 2017;30:37-43.
MacIntyre NR, Cook DJ, Ely EW, Jr., Epstein SK, Fink JB, Heffner JE, et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest 2001;120:375s-95s.
Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, et al. Weaning from mechanical ventilation. Eur Respir J 2007;29:1033-56.
Bai L, Duan J. Use of Cough Peak Flow Measured by a Ventilator to Predict Re-Intubation When a Spirometer Is Unavailable. Respir Care 2017;62:566-71.
McCool FD, Tzelepis GE. Dysfunction of the diaphragm. N Engl J Med 2012;366:932-42.
Goligher EC, Laghi F, Detsky ME, Farias P, Murray A, Brace D, et al. Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity. Intensive Care Med 2015;41:642-9.
Zhang B, Qin YZ. Comparison of pressure support ventilation and T-piece in determining rapid shallow breathing index in spontaneous breathing trials. Am J Med Sci 2014;348:300-5.
Pirompanich P, Romsaiyut S. Use of diaphragm thickening fraction combined with rapid shallow breathing index for predicting success of weaning from mechanical ventilator in medical patients. J Intensive Care 2018;6:6.
Ferrari G, De Filippi G, Elia F, Panero F, Volpicelli G, Aprà F. Diaphragm ultrasound as a new index of discontinuation from mechanical ventilation. Crit Ultrasound J 2014;6:8.
DiNino E, Gartman EJ, Sethi JM, McCool FD. Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation. Thorax 2014;69:423-7.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




