Energy expenditure in critically ill patient
DOI:
https://doi.org/10.54205/ccc.v30.259272Keywords:
Indirect calorimetry, Energy expenditure, Weight-based estimation, Energy deliveryAbstract
There are a variety of terms for energy expenditure. In severely ill patients, resting energy expenditure should be measured through indirect calorimetry or estimated using an equation or body weight. Although indirect calorimetry provides a more precise method of estimate, the measuring instrument has significant limitations and is not generally accessible in Thailand. Consequently, weight-based estimate is widespread, and it is currently the method that many societies suggest. For optimal results, energy supply should neither be excessive nor insufficient. The average energy delivery should account for between 70 and 85 percent of energy expenditures.
Downloads
References
Dvir D, Cohen J, Singer P. Computerized energy balance and complications in critically ill patients: an observational study. Clin Nutr 2006;25:37-44.
Villet S, Chiolero RL, Bollmann MD, Revelly JP, Cayeux RNM, Delarue J, et al. Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr 2005;24:502-9.
Chittawatanarat K, Chaiwat O, Morakul S, Kongsayreepong S. Outcomes of nutrition status assessment by Bhumibol Nutrition Triage/Nutrition Triage (BNT/NT) in multicenter THAI-SICU study J Med Assoc Thai 2016;99:S184-92.
Singer P, Anbar R, Cohen J, Shapiro H, Shalita-Chesner M, Lev S, et al. The tight calorie control study (TICACOS): a prospective, randomized, controlled pilot study of nutritional support in critically ill patients. Intensive Care Med 2011;37:601-9.
Oshima T, Berger MM, De Waele E, Guttormsen AB, Heidegger CP, Hiesmayr M, et al. Indirect calorimetry in nutritional therapy. A position paper by the ICALIC study group. Clin Nutr 2017;36:651-62.
Chittawatanarat K. Nutrition support in surgical ICU. In: Surgical critical care in practice. Edited by Chittawatanarat K: Chiang Mai, Faculty of Medicine, Chaing Mai University. 2017, pp 323-72.
da Rocha EE, Alves VG, da Fonseca RB. Indirect calorimetry: methodology, instruments and clinical application. Curr Opin Clin Nutr Metab Care 2006;9:247-56.
Chittawatanarat K, Morakul S, Thawitsri T, Thai Society of Critical Care Study group. Non cardio-pulmonary monitoring in Thai - ICU (ICU - RESOURCE I study). J Med Assoc Thai 2014;97:S31 - S7.
Chittawatanarat K, Tosanguan K, Chaikledkaew U. Knowledge gap of diagnosis and treatment of nutritional risk in hospital. Available at: http://www.hitap.net/documents/18954.
Moonen H, Beckers KJH, van Zanten ARH. Energy expenditure and indirect calorimetry in critical illness and convalescence: current evidence and practical considerations. J Intensive Care 2021;9:8.
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 2016;40:159-211.
Cerra FB, Benitez MR, Blackburn GL, Irwin RS, Jeejeebhoy K, Katz DP, et al. Applied nutrition in ICU patients. A consensus statement of the American College of Chest Physicians. Chest 1997;111:769-78.
Jacobs DG, Jacobs DO, Kudsk KA, Moore FA, Oswanski MF, Poole GV, et al. Practice management guidelines for nutritional support of the trauma patient. J Trauma 2004;57:660-78; discussion 79.
Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet P, Kazandjiev G, et al. ESPEN Guidelines on Enteral Nutrition: Intensive care. Clin Nutr 2006;25:210-23.
Singer P, Berger MM, Van den Berghe G, Biolo G, Calder P, Forbes A, et al. ESPEN Guidelines on Parenteral Nutrition: intensive care. Clin Nutr 2009;28:387-400.
Martindale RG, McClave SA, Vanek VW, McCarthy M, Roberts P, Taylor B, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition: Executive Summary. Crit Care Med 2009;37:1757-61.
Weimann A, Braga M, Carli F, Higashiguchi T, Hubner M, Klek S, et al. ESPEN guideline: Clinical nutrition in surgery. Clin Nutr 2017;36:623-50.
Compher C, Bingham AL, McCall M, Patel J, Rice TW, Braunschweig C, et al. Guidelines for the provision of nutrition support therapy in the adult critically ill patient: The American Society for Parenteral and Enteral Nutrition. JPEN J Parenter Enteral Nutr 2022;46:12-41.
Chittawatanarat K. Nutrition monitoring in surgical intensive care unit. In: Surgical critical care in practice. Edited by Chittawatanarat K: Chiang Mai, Faculty of Medicine, Chiang Mai University. 2017, pp 373 - 93.
Petros S, Horbach M, Seidel F, Weidhase L. Hypocaloric vs Normocaloric Nutrition in Critically Ill Patients: A Prospective Randomized Pilot Trial. JPEN J Parenter Enteral Nutr 2016;40:242-9.
Arabi YM, Aldawood AS, Haddad SH, Al-Dorzi HM, Tamim HM, Jones G, et al. Permissive Underfeeding or Standard Enteral Feeding in Critically Ill Adults. N Engl J Med 2015;372:2398-408.
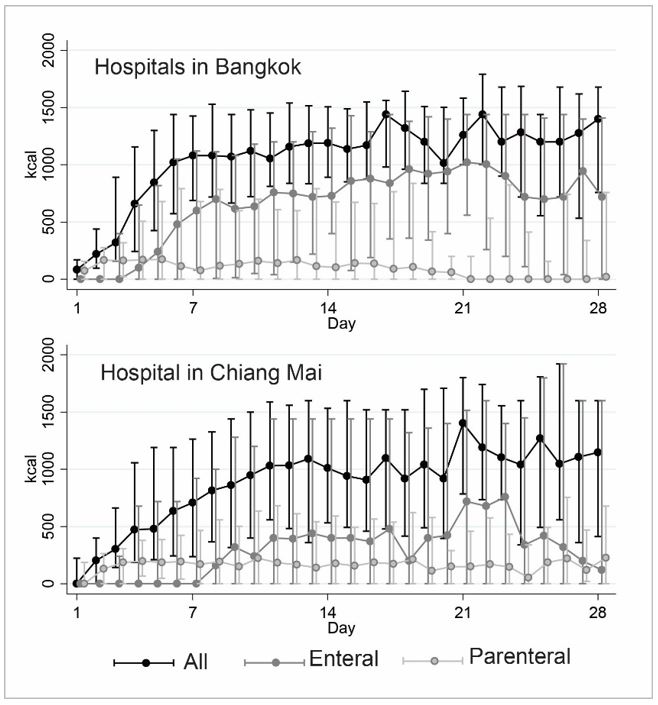
Chittawatanarat K, Chaiwat O, Morakul S, Kongsayreepong S. The differences of nutrition status, energy delivery and outcomes between metropolis and regional University-based Thai surgical intensive care units. J Med Assoc Thai 2016;99:S163-9.
Zusman O, Singer P. Resting energy expenditure and optimal nutrition in critical care: how to guide our calorie prescriptions. Crit Care 2017;21:128.
Zusman O, Theilla M, Cohen J, Kagan I, Bendavid I, Singer P. Resting energy expenditure, calorie and protein consumption in critically ill patients: a retrospective cohort study. Crit Care 2016;20:367.
Heyland DK, Cahill N, Day AG. Optimal amount of calories for critically ill patients: depends on how you slice the cake! Crit Care Med 2011;39:2619-26.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




