Prevention of contrast-associated acute kidney injury in critically-ill and high-risk preoperative patient: Protocol for a systematic review and network meta-analysis
Is CA-AKI preventable in ICU patients?
DOI:
https://doi.org/10.54205/ccc.v31.259642Keywords:
Critically-ill, Contrast-associated acute kidney injury, Network meta-analysisAbstract
Introduction: Limited information exists on preventing contrast-associated acute kidney injury (CA-AKI) in critically-ill patients. Extrapolating preventive strategies from non-critically-ill to critically-ill patients may jeopardize data validity. Therefore, it is imperative to evaluate the efficacy of preventive strategies by consolidating available clinical trial evidence through this systematic review and network meta-analysis (NMA).
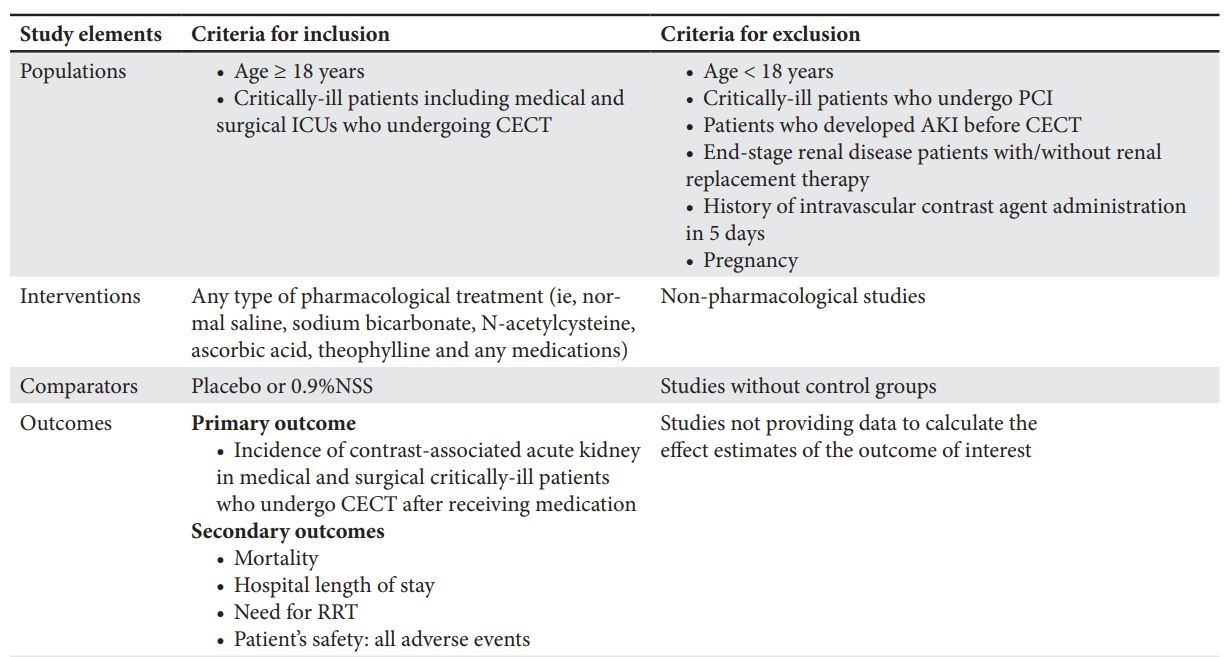
Methods and Analysis: We will conduct a comprehensive search of electronic databases, including PubMed, Embase, and Scopus, from their inception dates, with no language limitations. We will include both randomized trials and non-randomized studies that employ validated measurement tools to investigate the benefits of pharmacological interventions in patients undergoing contrast-enhanced computed tomography (CECT). The primary outcome of interest is the incidence of CA-AKI in medically and surgically critically-ill patients who receive medication prior to undergoing CECT. A pair of reviewers will independently perform risk of bias assessments and evaluate the strength of the evidence. We will employ a two-step approach, consisting of traditional pairwise meta-analysis and NMA. Utilizing a random-effects model, we will pool effect estimates as standardized weighted mean differences and odds ratios (ORs) with corresponding 95% confidence intervals (CIs) for continuous and categorical endpoints, respectively. We will assess both statistical and methodological heterogeneities. Preplanned subgroup analyses and univariate meta-regression will be conducted to quantify potential sources of heterogeneity. Evidence synthesis will be based on the effect size magnitudes, certainty of evidence, and surface under the cumulative ranking curve values.
Downloads
References
American College of Radiology (ACR) Committee on Drugs and Contrast Media. Manual on contrast media. https://www.acr.org/Clinical-Resources/Contrast-Manual 2021;Accessed April 22.
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO clinical practice guideline for acute kidney injury. 2012;2:1-138.
Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis 2002;39:930-6.
McCullough PA, Adam A, Becker CR, Davidson C, Lameire N, Stacul F, et al. Risk prediction of contrast-induced nephropathy. Am J Cardiol 2006;98:27K-36K.
Rihal CS, Textor SC, Grill DE, Berger PB, Ting HH, Best PJ, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation 2002;105:2259-64.
Wichmann JL, Katzberg RW, Litwin SE, Zwerner PL, De Cecco CN, Vogl TJ, et al. Contrast-Induced Nephropathy. Circulation 2015;132:1931-6.
James MT, Ghali WA, Tonelli M, Faris P, Knudtson ML, Pannu N, et al. Acute kidney injury following coronary angiography is associated with a long-term decline in kidney function. Kidney Int 2010;78:803-9.
Hoste E, Doom S, De Waele J, et al. Epidemiology of contrast-associated acute kidney injury in ICU patients: a retrospective cohort analysis. Intensive Care Med 2011;37:1921-31.
Sykes L, Nipah R, Kalra P, Green D. A narrative review of the impact of interventions in acute kidney injury. J Nephrol 2018;31:523-35.
Liu YH, Liu Y, Zhou YL, He PC, Yu DQ, Li LW, et al. Comparison of different risk scores for predicting contrast induced nephropathy and outcomes after primary percutaneous coronary intervention in patients with ST elevation myocardial infarction. Am J Cardiol 2016;117:1896-903.
Silver SA, Shah PM, Chertow GM, Harel S, Wald R, Harel Z. Risk prediction models for contrast induced nephropathy: systematic review. BMJ 2015;351:h4395.
Authors/Task Force m, Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014;35:2541-619.
Briguori C, Airoldi F, D'Andrea D, Bonizzoni E, Morici N, Focaccio A, et al. Renal Insufficiency Following Contrast Media Administration Trial (REMEDIAL): a randomized comparison of 3 preventive strategies. Circulation 2007;115:1211-7.
Merten G, Burgess W, Gray L, Holleman J, et al. Prevention of contrast-induced nephropathy with sodium bicarbonate: a randomized controlled trial. JAMA 2004;291:2328-34.
Ozcan EE, Guneri S, Akdeniz B, Akyildiz IZ, Senaslan O, Baris N, et al. Sodium bicarbonate, N-acetylcysteine, and saline for prevention of radiocontrast-induced nephropathy. A comparison of 3 regimens for protecting contrast-induced nephropathy in patients undergoing coronary procedures. A single-center prospective controlled trial. Am Heart J 2007;154:539-44.
Zoungas S, Ninomiya T, Huxley R, Cass A. Systematic review: sodium bicarbonate treatment regimens for the prevention of contrast-induced nephropathy. Ann Intern Med 2009;151:631-8.
Weisbord SD, Gallagher M, Jneid H, Garcia S, Cass A, Thwin SS, et al. Outcomes after Angiography with Sodium Bicarbonate and Acetylcysteine. N Engl J Med 2018;378:603-14.
Boscheri A, Weinbrenner C, Botzek B, Reynen K, Kuhlisch E, Strasser R. Failure of ascorbic acid to prevent contrast-media induced nephropathy in patients with renal dysfunction. Clin Nephrol 2007;68:279-86.
Dvorsak B, Kanic V, Ekart R, Bevc S, Hojs R. Ascorbic Acid for the prevention of contrast-induced nephropathy after coronary angiography in patients with chronic renal impairment: a randomized controlled trial. Ther Apher Dial 2013;17:384-90.
Spargias K, Alexopoulos E, Kyrzopoulos S, Iokovis P, Greenwood DC, Manginas A, et al. Ascorbic acid prevents contrast-mediated nephropathy in patients with renal dysfunction undergoing coronary angiography or intervention. Circulation 2004;110:2837-42.
Zhou L, Chen H. Prevention of contrast-induced nephropathy with ascorbic acid. Intern Med 2012;51:531-5.
Huber W, Eckel F, Hennig M, Rosenbrock H, et al. Prophylaxis of contrast material-induced nephropathy in patients in intensive care: acetylcysteine, theophylline, or both? A randomized study. Radiology 2006;239:793-804.
Higgins JPT, Thomas J, Chandler J. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). The Cochrane Collaboration 2022.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647.
Puhan MA, Schunemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ 2014;349:g5630.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898.
Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 2015;162:777-84.
Alway SE, Pereira SL, Edens NK, Hao Y, Bennett BT. beta-Hydroxy-beta-methylbutyrate (HMB) enhances the proliferation of satellite cells in fast muscles of aged rats during recovery from disuse atrophy. Exp Gerontol 2013;48:973-84.
IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol 2014;14:25.
Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34.
Higgins JP, Jackson D, Barrett JK, Lu G, Ades AE, White IR. Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Res Synth Methods 2012;3:98-110.
Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS One 2013;8:e76654.
Riley RD, Higgins JPT, Deeks JJ. Interpretation of random effects meta-analyses. BMJ 2011;342:d549.
Palli E, Makris D, Papanikolaou J, Garoufalis G, Zakynthinos E. Contrast-induced nephropathy in aged critically ill patients. Oxidative Medicine and Cellular Longevity 2014;2014:1-6.
Nikolakopoulou A, Higgins JPT, Papakonstantinou T, Chaimani A, Del Giovane C, Egger M, et al. CINeMA: An approach for assessing confidence in the results of a network meta-analysis. PLoS Med 2020;17:e1003082.
Chen H, Cohen P, Chen S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Communications in Statistics - Simulation and Computation 2010;39:860-4.
Cohen J. Statistical power analysis for the behavioral sciences 2nd ed. New York:Routledge 1988.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




