Use of Near-InfraRed Spectroscopy (NIRS) during Vascular Occlusion Test (VOT) for predicting an increase in oxygen consumption after fluid challenge in circulatory shock patients
Oxygen consumption responsiveness in fluid responder prediction method by bedside microcirculatory assessment tools
DOI:
https://doi.org/10.54205/ccc.v31.259970Keywords:
Circulatory failure, Fluid challenge, Fluid responder, Oxygen consumption responder, Near-infrared spectroscopy, Vascular occlusion testAbstract
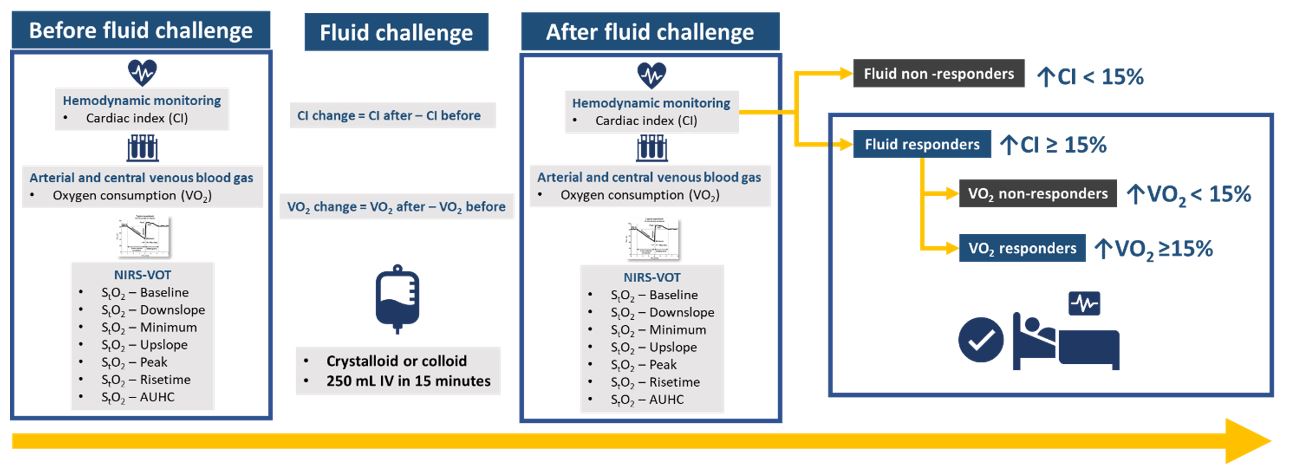
Background: The goal of fluid challenge (FC) is to increase cardiac output (CO) and oxygen delivery (DO2) (known as fluid responders) to correct tissue hypoxia. To optimize fluid administration, fluid challenge (FC) during dependence of oxygen consumption on oxygen delivery (VO2/DO2 dependency) would correct tissue hypoxia confirmed by an increase of oxygen consumption (VO2) and oxygen delivery (DO2) after FC (known as VO2 responders) and get more benefit from a reduction in tissue hypoxia. Markers of anaerobic metabolisms, such as blood lactate concentration or the ratio of venous-arterial CO2 tension difference (P(cv-a)CO2) over arterial-to-venous oxygen content difference (C(a-cv)O2), can predict VO2 responders but still have several limitations. Therefore, near-infrared spectroscopy (NIRS) has been developed to evaluate tissue perfusion, presented as tissue oxygen saturation (StO2), at the bedside. Combining StO2 with the vascular occlusive test (VOT) and introducing a short period of forearm ischemia is a non-invasive technique to examine microvascular alterations at the bedside. However, a study validating the ability of these variables to predict VO2 response has not been conducted.
Methods: We plan to conduct a single-center prospective study on circulatory failure patients. The cardiac index (CI), oxygen delivery (DO2), oxygen consumption (VO2), arterial lactate, central venous oxygen saturation (ScvO2), ratio of venous-arterial carbon dioxide tension to arterial-to-central venous oxygen content difference (P(cv-a)CO2/ C(a-cv)O2), and tissue oxygen saturation measured by near-infrared spectroscopy (NIRS) probe during vascular occlusion test variables (NIRS-VOT variables) will be collected before and after the fluid challenge.
Hypothesis: We hypothesize that markers of reactive hyperemia by NIRs will predict an increase in VO2 after FC in patients with circulatory shock.
Ethics: The study protocol has been approved by the ethics committee of the faculty of medicine, Ramathibodi Hospital, Mahidol University (COA. MURA2022/80).
Downloads
References
Ince C. Hemodynamic coherence and the rationale for monitoring the microcirculation. Crit Care. 2015;19 Suppl 3:S8.
Haupt MT, Gilbert EM, Carlson RW. Fluid loading increases oxygen consumption in septic patients with lactic acidosis. Am Rev Respir Dis. 1985;131:912-6.
Schumacker PT, Cain SM. The concept of a critical oxygen delivery. Intensive Care Med. 1987;13:223-9.
Vallet B. Pathophysiology of VO2/DO2 in Sepsis. In: Pinsky MR, editor. Applied Cardiovascular Physiology. Berlin, Heidelberg: Springer Berlin Heidelberg; 1997. p 185-96.
Shi R, Monnet X, Teboul JL. Parameters of fluid responsiveness. Curr Opin Crit Care. 2020;26:319-26.
Monnet X, Julien F, Ait-Hamou N, Lequoy M, Gosset C, Jozwiak M, et al. Lactate and venoarterial carbon dioxide difference/arterial-venous oxygen difference ratio, but not central venous oxygen saturation, predict increase in oxygen consumption in fluid responders. Crit Care Med. 2013;41:1412-20.
Mallat J, Lemyze M, Meddour M, Pepy F, Gasan G, Barrailler S, et al. Ratios of central venous-to-arterial carbon dioxide content or tension to arteriovenous oxygen content are better markers of global anaerobic metabolism than lactate in septic shock patients. Ann Intensive Care. 2016;6:10.
James JH, Luchette FA, McCarter FD, Fischer JE. Lactate is an unreliable indicator of tissue hypoxia in injury or sepsis. Lancet. 1999;354:505-8.
Mallat J, Lazkani A, Lemyze M, Pepy F, Meddour M, Gasan G, et al. Repeatability of blood gas parameters, PCO2 gap, and PCO2 gap to arterial-to-venous oxygen content difference in critically ill adult patients. Medicine (Baltimore). 2015;94:e415.
Creteur J, Carollo T, Soldati G, Buchele G, De Backer D, Vincent JL. The prognostic value of muscle StO2 in septic patients. Intensive Care Med. 2007;33:1549-56.
Pareznik R, Knezevic R, Voga G, Podbregar M. Changes in muscle tissue oxygenation during stagnant ischemia in septic patients. Intensive Care Med. 2006;32:87-92.
Gómez H, Torres A, Polanco P, Kim HK, Zenker S, Puyana JC, et al. Use of non-invasive NIRS during a vascular occlusion test to assess dynamic tissue O(2) saturation response. Intensive Care Med. 2008;34:1600-7.
Bezemer R, Lima A, Myers D, Klijn E, Heger M, Goedhart PT, et al. Assessment of tissue oxygen saturation during a vascular occlusion test using near-infrared spectroscopy: the role of probe spacing and measurement site studied in healthy volunteers. Crit Care. 2009;13 Suppl 5:S4.
Vincent J-L, Cecconi M, De Backer D. The fluid challenge. Critical Care. 2020;24:703.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29-36.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




