Restrictive fluid management and early fluid de-escalation versus usual care in critically ill patients: A feasibility trial protocol for the REDUCE randomized clinical trial
A feasibility trial protocol for the REDUCE randomized clinical trial
DOI:
https://doi.org/10.54205/ccc.v31.260808Keywords:
Restrictive fluid management, Circulatory shock, Vasopressor, Fluid balance, MortalityAbstract
Background: Fluid therapy is an essential therapeutic intervention for critically ill patients. Both fluid overload and hypovolemia are associated with poor outcomes. However, the fluid strategy in intensive care units is still controversial, and there is no consensus on using the fluid strategy in patients with circulatory shock.
Objectives: To compare the efficacy of protocol-based fluid-restrictive management versus standard care in critically ill patients with circulatory shock.
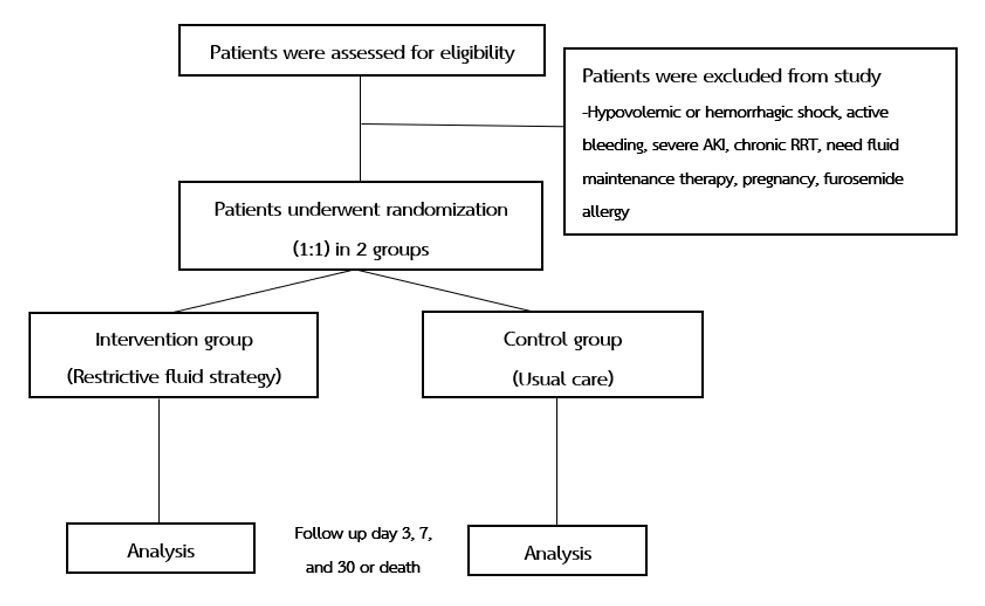
Methods: This is a single-center, feasibility-based, randomized, controlled trial in critically ill patients with circulatory shock receiving either fluid resuscitation or vasopressors in two medical ICUs at Siriraj Hospital. Eligible patients will be randomly allocated in a 1:1 ratio and placed in the restrictive fluid strategy (intervention) group or standard care (control) group. The primary outcome is accumulative fluid balance 72 hours after enrollment.
Conclusions: This study will evaluate the efficacy and safety of a protocol-based fluid restrictive strategy in critically ill patients who have circulatory shock and are receiving fluid resuscitation or vasopressors.
Downloads
References
Vincent JL. Fluid management in the critically ill. Kidney Int. 2019;96(1):52-57.
Malbrain M L. N. G., Regenmortel NV, Saugel B, Tavernier BD, Van Gaal PJ, Joannes-Boyau O, Teboul JL, et al. Principles of fluid management and stewardship in septic shock: it is time to consider the four D’s and the four phases of fluid therapy. Ann Intensive Care. 2018;8:66.
Claure-Del Granado R, Mehta RL. Fluid overload in the ICU: evaluation and management. BMC Nephrology. 2016;17:109.
Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, et al. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;76(4):422–7.
Nisula S, Kaukonen KM, Vaara ST, Korhonen AM, Poukkanen M, Karlsson S, et al. Incidence, risk factors and 90-day mortality of patients with acute kidney injury in Finnish intensive care units: the FINNAKI study. Intensive Care Med. 2013;39:420–428.
Vaara ST, Korhonen AM, Kaukonen KM, Sara Nisula1, Inkinen Q, Hoppu S, et al. Fluid overload is associated with an increased risk for 90-day mortality in critically ill patients with renal replacement therapy: data from the prospective FINNAKI study. Crit Care. 2012; 16(5): R197.
Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, et al. Comparison of two fluid management strategies in acute lung injury. N Engl J Med. 2006;354:2564–2575.
Myles PS, Bellomo R, Corcoran T, Forbes A, Peyton P, Story D. Restrictive versus Liberal Fluid Therapy for Major Abdominal Surgery. N Engl J Med 2018;378:2263-2274.
Vaara ST, Ostermann M, Bitker L, Schneider A, Poli E, Hoste E, et al. Restrictive fluid management versus usual care in acute kidney injury (REVERSE-AKI): a pilot randomized controlled feasibility trial. Intensive Care Med. 2021;47(6):665-673.
Meyhoff TS, Hjortrup PB, Wetterslev J, Sivapalan P, Laake JH, et al. Restriction of Intravenous fluid in ICU patients with septic shock (CLASSIC). N Engl J Med. 2022;386:2459-70.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




