Effect of early post-extubation high-flow nasal cannula versus conventional low-flow oxygen therapy on reintubation in postoperative patients from prolonged general anesthesia at surgical ICU: A randomized clinical trial (Protocol)
High versus low flow oxygen therapy after extubation in prolonged general anesthesia patients
DOI:
https://doi.org/10.54205/ccc.v31.260850Keywords:
High flow nasal cannula, Oxygen therapy, Reintubation, Postoperative pulmonary complications, Prolonged general anesthesiaAbstract
Background: The main concerns following general anesthesia, especially if it lasts longer than 4 hours, are postoperative pulmonary complications, including hypoxemia, lung atelectasis, and acute respiratory failure requiring reintubation. To avoid these complications, postoperative extubation with respiratory support is crucial. The high-flow nasal cannula (HFNC) increases end-expiratory lung volume and reduces the work of breathing to improve oxygenation by delivering a flow-dependent positive airway pressure. The advantages of using HFNC to prevent reintubation have been demonstrated in patients undergoing cardiothoracic surgery. Our target population's information is still deficient, and our trial is set up to uncover this proof.
Objectives: To evaluate the effect of high-flow nasal cannula (HFNC) versus low-flow nasal cannula on the reintubation rate and clinical outcomes in the early post-extubation adult who has prolonged general anesthesia for non-cardiothoracic and non-neuro surgery that requires surgical ICU admission.
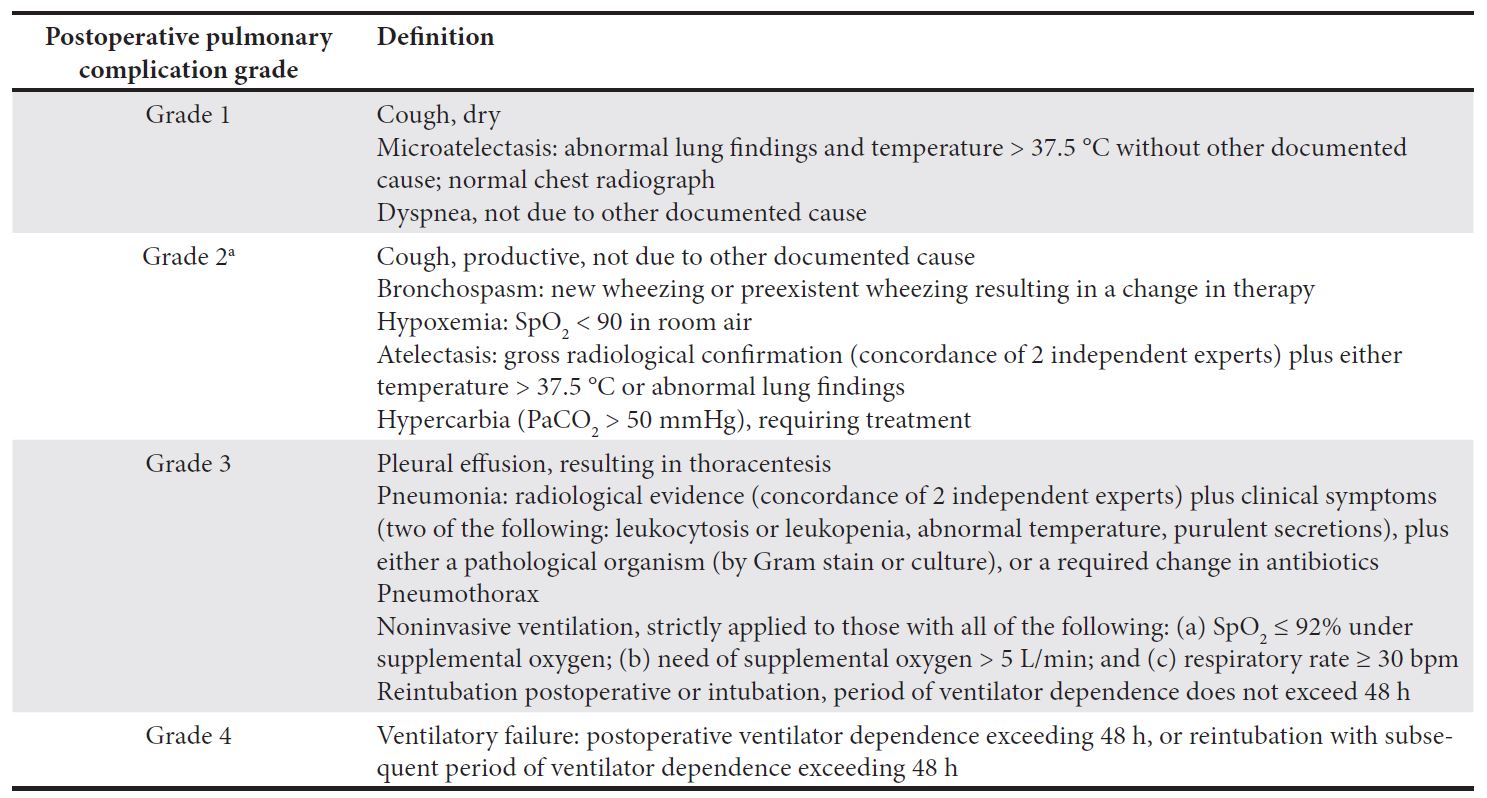
Methods: In this study, 260 patients with an intermediate to high risk of postoperative pulmonary complications following non-cardiothoracic surgery and non-neurosurgery that required general anesthesia for longer than 4 hours were randomly assigned to receive either a high-flow nasal cannula (HFNC) or a low-flow nasal cannula after extubation. The primary outcome indicator is the reintubation rate within 72 hours of tracheal extubation. Postoperative pulmonary complications, the length of stay in the ICU and hospital, and mortality are considered secondary outcome measures.
Conclusions: This study is an investigator-initiated randomized controlled trial powered to test the hypothesis that early application of a high-flow nasal cannula probably reduces the reintubation rate in patients in SICUs with prolonged durations of general anesthesia.
Downloads
References
Futier E, Constantin J-M, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369(5):428-37.
Futier E, Paugam-Burtz C, Constantin J-M, Pereira B, Jaber S. The OPERA trial-comparison of early nasal high flow oxygen therapy with standard care for prevention of postoperative hypoxemia after abdominal surgery: study protocol for a multicenter randomized controlled trial. Trials. 2013;14(1):1-7.
Futier E, Paugam-Burtz C, Godet T, Khoy-Ear L, Rozencwajg S, Delay J-M, et al. Effect of early postextubation high-flow nasal cannula vs conventional oxygen therapy on hypoxaemia in patients after major abdominal surgery: a French multicentre randomised controlled trial (OPERA). Intensive Care Med. 2016;42(12):1888-98.
Lu Z, Chang W, Meng S, Xue M, Xie J, Xu J, et al. The effect of high-flow nasal oxygen therapy on postoperative pulmonary complications and hospital length of stay in postoperative patients: a systematic review and meta-analysis. J Intensive Care Med. 2020;35(10):1129-40.
François S, Benoit B, Pascal P, Saida R-D, Anne M, Bertrand D, et al. High-flow nasal oxygen vs noninvasive positive airway pressure in hypoxemic patients after cardiothoracic surgery: A randomized clinical trial. JAMA. 2015;313(23):2331-9.
Routh JC, Bacon DR, Leibovich BC, Zincke H, Blute ML, Frank I. How long is too long? The effect of the duration of anaesthesia on the incidence of non‐urological complications after surgery. BJU international. 2008;102(3):301-4.
Mazo V, Sabate S, Canet J, Gallart L, De Abreu MG, Belda J, Langeron O, Hoeft A, Pelosi P. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology. 2014;121(2):219-31.
Fernandez-Bustamante A, Frendl G, Sprung J, Kor DJ, Subramaniam B, Ruiz RM, Lee JW, Henderson WG, Moss A, Mehdiratta N, Colwell MM. Postoperative pulmonary complications, early mortality, and hospital stay following noncardiothoracic surgery: a multicenter study by the perioperative research network investigators. JAMA surgery. 2017;152(2):157-66.
Gonzalo H, Concepción V, Laura C, Rafael C, Paloma G, Alfonso C. Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high risk patients a randomized clinical trial. JAMA. 2016;316(15):1565-74.
Lu Z, Chang W, Meng S-S, Zhang X, Xie J, Xu J-Y, et al. Effect of high-flow nasal cannula oxygen therapy compared with conventional oxygen therapy in postoperative patients: a systematic review and meta-analysis. BMJ open. 2019;9(8):e027523.
Ni Y-N, Luo J, Yu H, Liu D, Liang B-M, Yao R, et al. Can high-flow nasal cannula reduce the rate of reintubation in adult patients after extubation? A meta-analysis. BMC Pulm Med. 2017;17(1):1-10.
Ansari BM, Hogan MP, Collier TJ, Baddeley RA, Scarci M, Coonar AS, et al. A randomized controlled trial of high-flow nasal oxygen (Optiflow) as part of an enhanced recovery program after lung resection surgery. The Annals of thoracic surgery. 2016;101(2):459-64.
Gaspari R, Spinazzola G, Ferrone G, Soave PM, Pintaudi G, Cutuli SL, et al. High-flow nasal cannula versus standard oxygen therapy after extubation in liver transplantation: a matched controlled study. Respir Care. 2020;65(1):21-8.
Hernández G, Vaquero C, González P, Subira C, Frutos-Vivar F, Rialp G, et al. Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA. 2016;315(13):1354-61.
Li XF, Jiang D, Jiang YL, Yu H, Jiang JL, He LL, Yang XY, Yu H. PROtective Ventilation with a low versus high Inspiratory Oxygen fraction (PROVIO) and its effects on postoperative pulmonary complications: protocol for a randomized controlled trial. Trials. 2019;20(1):1-0.
Siempos II, Xourgia E, Ntaidou TK, Zervakis D, Magira EE, Kotanidou A, Routsi C, Zakynthinos SG. Effect of early vs. delayed or no intubation on clinical outcomes of patients with COVID-19: an observational study. Frontiers in medicine. 2020;7:614152.
Miskovic A, Lumb AB. Postoperative pulmonary complications. BJA: British Journal of Anaesthesia. 2017;118(3):317-34.
Rujirojindakul P, Geater AF, McNeil EB, Vasinanukorn P, Prathep S, Asim W, Naklongdee J. Risk factors for reintubation in the post-anaesthetic care unit: a case–control study. British journal of anaesthesia. 2012;109(4):636-42.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




