Cerebral oximetry and autoregulation monitoring in shock patients
Cerebral oximetry and autoregulation monitoring in shock
DOI:
https://doi.org/10.54205/ccc.v31.260918Keywords:
Near-infrared spectroscopy, Regional cerebral oxygen saturation, Cerebral oximetry index, Cerebral autoregulation, Shock, Tissue perfusionAbstract
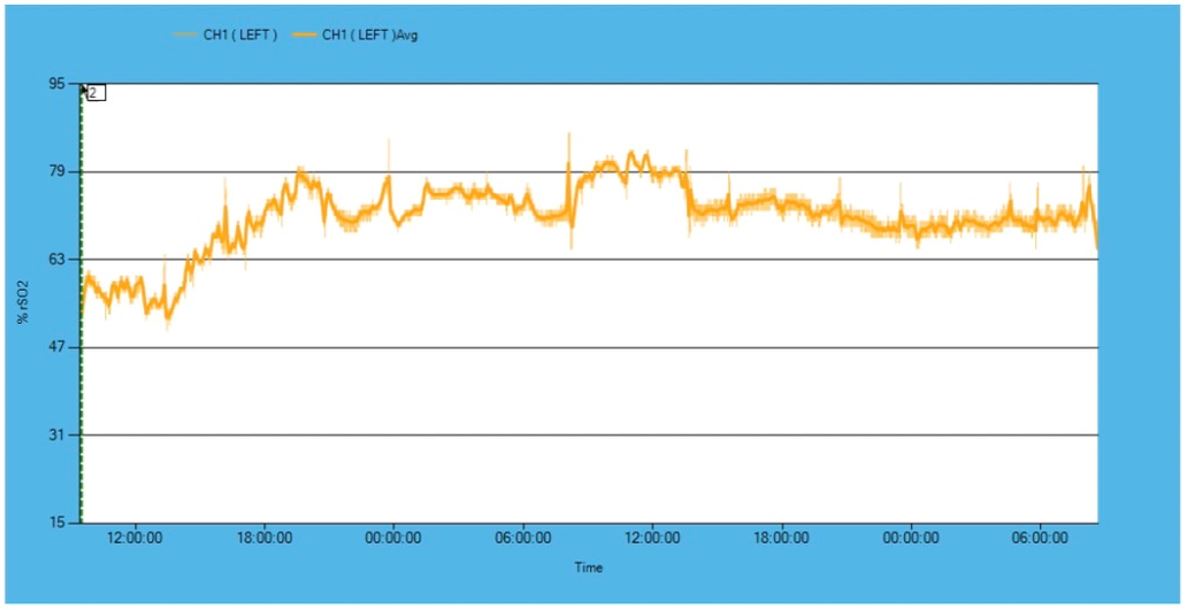
Background: Data on regional cerebral oxygen saturation (rSO2) and cerebral autoregulation monitoring in shock patients are limited. This study aimed to find the optimal range of rSO2 and cerebral oximetry index (COx), an autoregulation index correlated with adequate tissue perfusion determined by standard clinical and laboratory assessment.
Method: We plan to monitor cerebral oximetry using near-infrared spectroscopy in shock patients admitted to the medical intensive care unit (MICU) at Siriraj Hospital. The rSO2 are continuously recorded for 72 hours [48] after admission or 24 hours after cessation of vasopressor infusion. The COx is calculated from the correlation coefficient between rSO2 and MAP. Data on patient demographics, treatments, physiologic parameters, and outcomes are recorded. The primary objective is to identify the optimal rSO2 and COx correlated with adequate tissue perfusion assessed by the current standard method. Adequate tissue perfusion as is defined as MAP ≥65 mmHg and two of the following criteria: urine ≥0.5 ml/kg/hour, capillary refill time ≤3 seconds, improvement in consciousness, lactate reduction ≥10% in 1 hour, serum lactate <2 mmol/L, or central venous oxygen saturation (ScVO2) ≥70%. Since the optimal values of rSO2 and COx in shock patients are unknown, we are unable to perform the sample size calculation. Thus, for this study, we plan to collect data on rSO2 and COx in 30 patients.
Hypothesis: We hypothesize that the values of rSO2 and COx are different between patients with adequate and inadequate tissue perfusion.
Ethics statement: The study was reviewed and approved by the Human Research Protection Unit of Siriraj Hospital, Mahidol University (certificate of approval no. si 410/2022).
Downloads
References
Evans L, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181-1247.
Angkasekwinai N, Rattanaumpawan P, Thamlikit kul V. Epidemiology of sepsis in Siriraj Hospital 2007. J Med Assoc Thai. 2009;92(2): S68-78.
Jackson JC, Pandharipande PP, Girard TD, Brummel NE, Thompson JL, Hughes CG, et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longi- tudinal cohort study. Lancet Respir Med. 2014;2(5):369-79.
Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. Jama. 2010;304(16):1787-94.
Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293-304.
Kato R, Pinsky MR. Personalizing blood pressure management in septic shock. Ann Intensive Care. 2015;5(1):41.
Kenneth M. Brady, Aaron Hudson, Ryan Hood, Bruno DeCaria, Choy Lewis, Charles W. Hogue. Personalizing the definition of hypotension to protect the brain. Anesthesiology 2020; 132:170–179.
Ghosh A, Elwell C, Smith M. Review article: cerebral near-infrared spectroscopy in adults: a work in progress. Anesth Analg. 2012;115(6): 1373-83.
Samra SK, Dy EA, Welch K, Dorje P, Zelenock GB, Stanley JC. Evaluation of a cerebral oximeter as a monitor of cerebral ischemia during carotid endarterectomy. Anesthesiology. 2000;93(4):964-70.
Al-Rawi PG, Kirkpatrick PJ. Tissue oxygen index: thresholds for cerebral ischemia using near-infrared spectroscopy. Stroke. 2006;37(11):2720-5.
Murkin JM, Adams SJ, Novick RJ, Quantz M, Bainbridge D, Iglesias I, et al. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg. 2007;104(1):51-8.
Wong JK, Smith TN, Pitcher HT, Hirose H, Cavarocchi NC. Cerebral and lower limb near-infrared spectroscopy in adults on extracorporeal membrane oxygenation. Artif Organs. 2012;36(8):659-67.
Rivera-Lara L, Zorrilla-Vaca A, Geocadin RG, Healy RJ, Ziai W, Mirski MA. Cerebral autoregulation-oriented therapy at the bedside: A compre-hensive review. Anesthesiology. 2017;126(6):1187-99.
Rivera-Lara L, Geocadin R, Zorrilla-Vaca A, Healy R, Radzik BR, Palmisano C, et al. Validation of near-infrared spectroscopy for monitoring cerebral autoregulation in Comatose patients. Neurocrit Care. 2017;27(3):362-9.
Ono M, Zheng Y, Joshi B, Sigl JC, Hogue CW. Validation of a stand-alone near-infrared spectroscopy system for monitoring cerebral autoregulation during cardiac surgery. Anesth Analg. 2013;116(1):198-204.
Hogue CW, Levine A, Hudson A, Lewis C. Clinical applications of near-infrared spectroscopy monitoring in cardiovascular surgery. Anesthesio-logy. 2021;134(5):784-791.
Le Roux PD, Levine JM, Kofke WA, editors. Monitoring in neurocritical care. Philadelphia: Elsevier; 2013.
Erdoes G, Rummel C, Basciani RM, Verma R, Carrel T, Banz Y, Eberle B, Schroth G. Limitations of current near-infrared spectroscopy config-uration in detecting focal cerebral ischemia during cardiac surgery: An observational case-series study. Artif Organs. 2018;42(10):1001-1009.
Oddo M, Bosel J. Monitoring of brain and systemic oxygenation in neurocritical care patients. Neurocrit Care. 2014;21 Suppl 2: S103-20.
Das D, Mitra K, Das S. Brain Co-oximetry: A useful non-invasive parameter adjuvant to standard perfusion parameters in septic shock. J Anesth Clin Res. 2021; 12:987.
Rivera-Lara L, Zorrilla-Vaca A, Geocadin RG, Healy RJ, Ziai W, Mirski MA. Cerebral autoregulation-oriented therapy at the bedside: A compre-hensive review. Anesthesiology. 2017;126(6):1187-99.
Lee KF, Wood MD, Maslove DM, Muscedere JG, Boyd JG. Dysfunctional cerebral autoregulation is associated with delirium in critically ill adults. J Cereb Blood Flow Metab. 2019;39(12):2512-2520.
Rosenblatt K, Walker KA, Goodson C, Olson E, Maher D, Brown CHt, et al. Cerebral autoregulation-guided optimal blood pressure in sepsis-associated encephalopathy: A case series. J Intensive Care Med. 2020; 35(12):1453-64.
Petersen NH, Silverman A, Strander SM, Kodali S, Wang A, Sansing LH, et al. Fixed compared with autoregulation-oriented blood pressure thres-holds after mechanical thrombectomy for ischemic stroke. Stroke. 2020; 51(3):914-21.
Ameloot K, Genbrugge C, Meex I, Jans F, Boer W, Vander Laenen M, et al. An observational near-infrared spectroscopy study on cerebral autoregulation in post-cardiac arrest patients: time to drop 'one-size-fits-all' hemodynamic targets Resuscitation. 2015; 90:121-6.
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40(12):1795-815.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1(7905):480–4.
Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, et al. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013 Dec 5;369(23):2197-206.
Girard TD, Exline MC, Carson SS, Hough CL, Rock P, Gong MN, et al. Haloperidol and ziprasidone for treatment of delirium in critical illness. N Engl J Med. 2018;379(26):2506-2516.
Permpikul C, Tongyoo S, Viarasilpa T, Trainarongsakul T, Chakorn T, Udompanturak S. Early use of norepinephrine in septic shock resuscitation (CENSER). A randomized trial. Am J Respir Crit Care Med. 2019;199(9):1097-1105.
Walley KR. Shock. In: Hall JB, Schmidt GA, Kress JP, editors. Principles of critical care, 4th ed. New York: McGraw-Hill, 2015, 249-262.
Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013;369(18): 1726-34.
Harjola VP, Mebazaa A, Celutkiene J, Bettex D, Bueno H, Chioncel O, et al. Contemporary management of acute right ventricular failure. Eur J Heart Fail. 2016;18(3):226-41.
Cannon JW. Hemorrhagic shock. N Engl J Med. 2018;378(4):370-379.
Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003;349(7):684-90.
van Diepen S, Katz JN, Albert NM, Henry TD, Jacobs AK, Kapur NK, et al. Contemporary management of cardiogenic shock: A scientific statement from the American heart association. Circulation. 2017;136(16): e232-e268.
Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the abdominal compartment syndrome. Intensive Care Med. 2013;39(7):1190-206.
Chaohui Lian, et al. Comparison of basic regional cerebral oxygen saturation values in patients of different ages: A pilot study. Journal of international medical research. 2020; 48(8) 1-9.
Kenneth M. Brady, MD., et al. Continuous time-domain analysis of cerebrovascular autoregulation using near-infrared spectrometry. Stroke. 2007; 38:2818-2825.
Kamal Ajam, et al. Reliability of the Cerebral Performance Category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort study. Trauma, resuscitation and emergency medicine. 2011; 19:38.
Jones AE, Trzeciak S, Kline JA. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit Care Med. 2009;37(5):1649–54.
Pipanmekaporn T, Wongpakaran N, Mueankwan S, Dendumrongkul P, Chittawatanarat K, Khongpheng N, et al. Validity and reliability of the Thai version of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Clin Interv Aging. 2014; 9:879–85.
M. Luwis et al. Determing sample size for progression criteria for pragmatic pilot RCTs: the hypothesis test strikes back. Pilot and Feasibility Studies. 2021; 7:40.
DeSai C, Hays Shapshak A. Cerebral Ischemia. [Updated 2022 May 2]. In: StatPearls [Internet].
Deschamps A, Lambert J, Couture P, et al. Reversal of decreases in cerebral saturation in high-risk cardiac surgery. J Cardiothorac Vasc Anesth. 2013; 27(6): 1260-1266.
Schoen J, Husemann L, Tiemeyer C, et al. Cognitive function after sevoflurane- vs propofol-based anaesthesia for on-pump cardiac surgery: a randomized controlled trial. Br J Anaesth. 2011;106(6): 840-850.
Kerry L. Tomlin, et al. Detection of critical cerebral desaturation thresholds by three regional oximeters during hypoxia: a pilot study in healthy volunteers. BMC Anesthesiology. 2017;17(6).
Kristine E Mulier, et al. Near-infrared spectroscopy in patients with severe sepsis: correlation with invasive hemodynamic measurements. Surg Infect (Larchmt). 2008;9(5):515-9.
Mathews Jacob, et al. Correlation between cerebral co-oximetry (rSO2) and outcomes in traumatic brain injury cases: A prospective, observational study. Medical Journal Armed Forces India. 2019;75(2): 190-196.
Carrie M. Goodson, MD, et al. Cerebral blood flow autoregulation in sepsis for the intensivist: why its monitoring may be the future of individualized care. Journal of Intensive Care Medicine. 2018; 33(2): 63-73
Cheng Ni, et al. Cerebral oxygen saturation after multiple perioperative influential factors predict the occurrence of postoperative cognitive dysfunction. BMC Anesthesiol. 2015; 15:156.
Masahiro Ono, et al. Duration and magnitude of blood pressure below cerebral autoregulation threshold during cardiopulmonary bypass is associated with major morbidity and operative mortality. J Thorac Cardiovasc Surg. 2014;147(1): 483-489.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




