Positive end-expiratory pressure in acute respiratory distress syndrome; where have we been, where are we going?
PEEP setting in ARDS
DOI:
https://doi.org/10.54205/ccc.v31.262904Keywords:
ARDS, Lung compliance, Oxygenation, PEEP, Recruitment, Respiratory system complianceAbstract
ARDS is a heterogenous syndrome with a high mortality rate and limited therapeutic strategies. PEEP is routinely applied to these patients as a part of a protective lung ventilation strategy because getting it right helps optimize respiratory system compliance and improve oxygenation. However, if the PEEP is too low or too high, it may cause harm. Large clinical trials, focusing on patients with ARDS, have generally compared strategies designed to deliver low PEEP with those designed to deliver higher PEEP. No superior strategy has emerged, perhaps because these studies did not stratify patients based on their likely response to high or low PEEP. Nevertheless, the best strategy to identify optimal PEEP remains controversial, despite many large studies over the past 50 years. In the modern era of personalized medicine, perhaps our PEEP strategy should not be high PEEP or low PEEP but individualized PEEP. In this manuscript, we review the physiological effects of PEEP and the various methods studied and available to determine optimal PEEP at the bedside, providing a guide for physicians who regularly manage mechanically ventilated patients and highlighting new avenues for research.
Downloads
References
Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet. 1967;290(7511):319–23.
Web HH and Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. protection by positive end-expiratory pressure. Am Rev Respir Dis. 1974,110(5):556-65.
Muscedere JG, Mullen JB, Gan K, Slutsky AS. Tidal ventilation at low airway pressures can augment lung injury. Am J Resp Crit Care. 1994;149(5):1327–34.
Weigelt JA, Mitchell RA, Snyder WH. Early positive end-expiratory pressure in the adult respiratory distress syndrome. Arch Surg. 1979;114(4):497–501.
Cove ME, Pinsky MR, Marini JJ. Are we ready to think differently about setting PEEP? Crit Care. 2022;26(1):222.
Grieco DL, Bongiovanni F, Dell’Anna AM, Antonelli M. Why compliance and driving pressure may be inappropriate targets for PEEP setting during ARDS. Crit Care. 2022;26(1):234.
Gattinoni L, Marini JJ. In search of the Holy Grail: identifying the best PEEP in ventilated patients. Intensive Care Med. 2022;48(6):728–31.
Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, et al. Higher versus Lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. NEJM. 2004;351(4):327–36.
Meade MO, Cook DJ, Guyatt GH, Slutsky AS, Arabi YM, Cooper DJ, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299(6):637–45.
Mercat A, Richard JCM, Vielle B, Jaber S, Osman D, Diehl JL, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299(6):646–55.
Cavalcanti AB, Suzumura ÉA, Laranjeira LN, Paisani DDM, Damiani LP, Guimarães HP, et al. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318(14):1335.
Hodgson CL, Cooper DJ, Arabi Y, King V, Bersten A, Bihari S, et al. Maximal recruitment open lung ventilation in acute respiratory distress syndrome (PHARLAP). A phase ii, multicenter randomized controlled clinical trial. Am J Resp Crit Care. 2019;200(11):1363–72.
Beitler JR, Sarge T, Banner-Goodspeed VM, Gong MN, Cook D, Novack V, et al. Effect of titrating positive end-expiratory pressure (PEEP) with an esophageal pressure–guided strategy vs an empirical high PEEP-Fio2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome. JAMA. 2019;321(9):846–57.
Boros SJ. Variations in inspiratory: expiratory ratio and airway pressure wave form during mechanical ventilation: The significance of mean airway pressure. J Pediatrics. 1979;94(1):114–7.
Gullberg N, Winberg P, Selldén H. Changes in mean airway pressure during HFOV influences cardiac output in neonates and infants. Acta Anaesthesio Scand. 2004;48(2):218–23.
Shapiro BA, Cane RD, Harrison RA. Positive end-expiratory pressure therapy in adults with special reference to acute lung injury. Crit Care Med. 1984;12(2):127–41.
Duncan AW, Oh TE, Hillman DR. PEEP and CPAP. Anaesth Intens Care. 1986;14(3):236–50.
He H, Chi Y, Long Y, Yuan S, Frerichs I, Möller K, et al. Influence of overdistension/recruitment induced by high positive end-expiratory pressure on ventilation–perfusion matching assessed by electrical impedance tomography with saline bolus. Crit Care. 2020;24(1):586.
Stokke DB. Review: Artifical ventilation with positive end-expiratory pressure (PEEP). Eur J Inten Care Med. 1976;2(2):77–85.
Villar J. The use of positive end-expiratory pressure in the management of acute respiratory failure. Minerva anestesiol. 2005;71(6):265-72
Gattinoni L, Collino F, Maiolo G, Rapetti F, Romitti F, Tonetti T, et al. Positive end-expiratory pressure: how to set it at the individual level. Ann Transl Med. 2017;5(14):288–288.
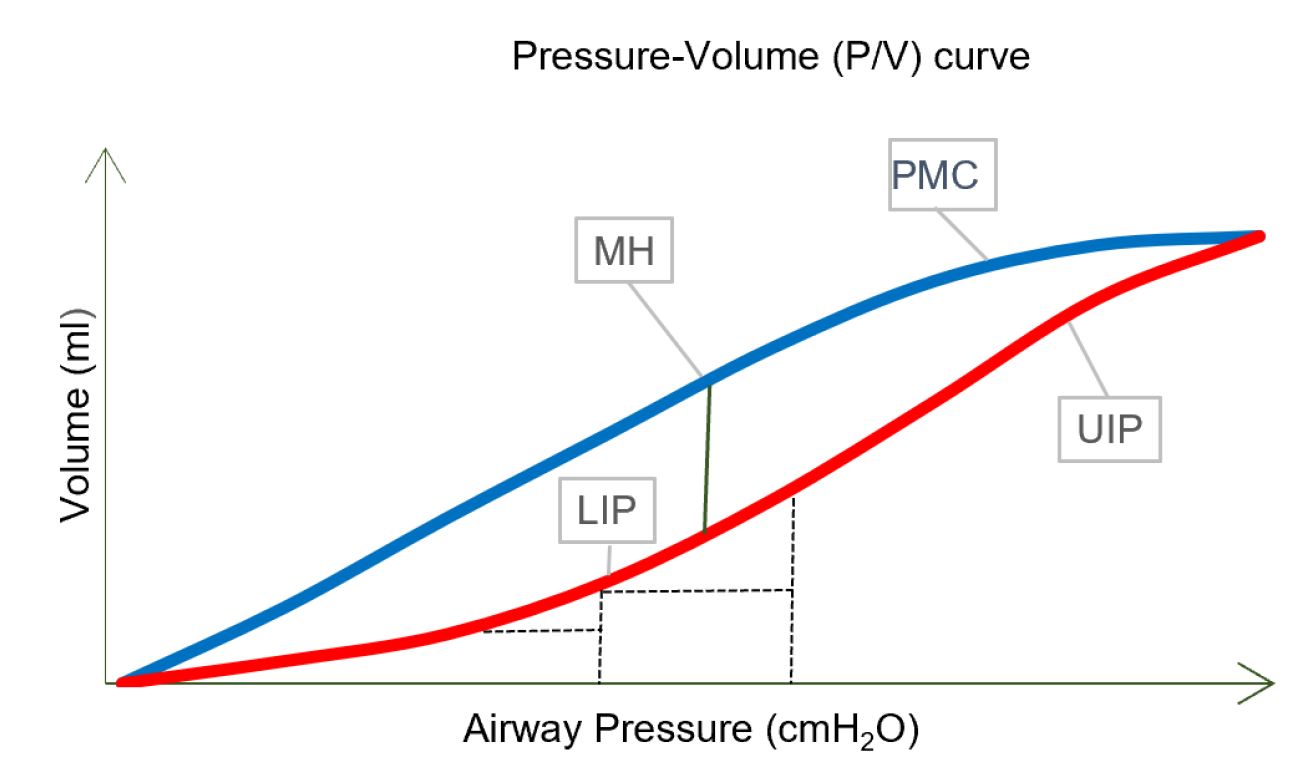
Maggiore SM, Richard JC, Brochard L. What has been learnt from P/V curves in patients with acute lung injury/acute respiratory distress syndrome. Eur Respir J Suppl. 2003;42:22s–6s.
Blanch L, López-Aguilar J, Villagrá A. Bedside evaluation of pressure–volume curves in patients with acute respiratory distress syndrome. Curr Opin Crit Care. 2007;13(3):332–7.
Scaramuzzo G, Spadaro S, Waldmann AD, Böhm SH, Ragazzi R, Marangoni et al. Heterogeneity of regional inflection points from pressure-volume curves assessed by electrical impedance tomography. Crit Care. 2019;23(1):119.
Prange HD. Laplace’s law and the alveolus: a misconception of anatomy and a misapplication of physics. Adv Physiol Educ. 2003;27(1):34–40.
Zucker AR, Holm BA, Crawford GP, Ridge K, Wood LD, Sznajder JI. PEEP is necessary for exogenous surfactant to reduce pulmonary edema in canine aspiration pneumonitis. J Appl Physiol. 1992;73(2):679–86.
Gattinoni L, Carlesso E, Cadringher P, Valenza F, Vagginelli F, Chiumello D. Physical and biological triggers of ventilator-induced lung injury and its prevention. Eur Respir J. 2003;22(Supplement 47):15s–25s.
Pinsky MR. the effects of mechanical ventilation on the cardiovascular system. Crit Care Clin. 1990;6(3):663–78.
Peters J. Mechanical ventilation with PEEP – a unique therapy for failing hearts. Intensive Care Med. 1999;25(8):778–80.
Luecke T, Pelosi P. Clinical review: Positive end-expiratory pressure and cardiac output. Crit Care. 2005;9(6):607–21.
Nieman GF, Paskanik AM, Bredenberg CE. Effect of positive end-expiratory pressure on alveolar capillary perfusion. J Thorac Cardiovasc Surg. 1988;95(4):712–6.
Çoruh B, Luks AM. Positive end-expiratory pressure. When more may not be better. Ann Am Thorac Soc. 2014;11(8):1327–31.
Protti A, Andreis DT, Milesi M, Iapichino GE, Monti M, Comini B, et al. Lung anatomy, energy load, and ventilator-induced lung injury. Intensive Care Med Exp. 2015;3(1):34.
Gattinoni L, Pesenti A. The concept of “baby lung.” Intens Care Med. 2005;31(6):776–84.
ARDS Network; Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. NEJM. 2000;342(18):1301–8.
Grasso S, Fanelli V, Cafarelli A, Anaclerio R, Amabile M, Ancona G, et al. Effects of high versus low positive end-expiratory pressures in acute respiratory distress syndrome. Am J Resp Crit Care. 2005;171(9):1002–8.
Calfee CS, Delucchi K, Parsons PE, Thompson BT, Ware LB, Matthay MA, et al. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med. 2014;2(8):611–20.
Terragni PP, Rosboch G, Tealdi A, Corno E, Menaldo E, Davini O, et al. Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Resp Crit Care. 2007;175(2):160–6.
Hodgson CL, Tuxen DV, Davies AR, Bailey MJ, Higgins AM, Holland AE, et al. A randomised controlled trial of an open lung strategy with staircase recruitment, titrated PEEP and targeted low airway pressures in patients with acute respiratory distress syndrome. Crit Care. 2011;15(3):R133.
Kassis EB, Loring SH, Talmor D. Should we titrate peep based on end-expiratory transpulmonary pressure?—yes. Ann Transl Med. 2018;6(19):390–390.
Talmor D, Sarge T, Malhotra A, O’Donnell CR, Ritz R, Lisbon A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. NEJM. 2008;359(20):2095–104.
Kassis EB, Talmor D. Clinical application of esophageal manometry: how I do it. Crit Care. 2021;25(1):6.
Sarge T, Baedorf-Kassis E, Banner-Goodspeed V, Novack V, Loring SH, Gong MN, et al. Effect of esophageal pressure–guided positive end-expiratory pressure on survival from acute respiratory distress syndrome: a risk-based and mechanistic reanalysis of the EPVent-2 Trial. Am J Resp Crit Care. 2021;204(10):1153–63.
Albaiceta GM, Taboada F, Parra D, Luyando LH, Calvo J, Menendez R, et al. Tomographic study of the inflection points of the pressure–volume curve in acute lung injury. Am J Resp Crit Care. 2004;170(10):1066–72.
Demory D, Arnal JM, Wysocki M, Donati S, Granier I, Corno G, et al. Recruitability of the lung estimated by the pressure volume curve hysteresis in ARDS patients. Intensive Care Med. 2008;34(11):2019.
Koefoed‐Nielsen J, Andersen G, Barklin A, Bach A, Lunde S, Tønnesen E, et al. Maximal hysteresis: a new method to set positive end‐expiratory pressure in acute lung injury? Acta Anaesthesiol Scand. 2008;52(5):641–9.
Grasso S, Terragni P, Mascia L, Fanelli V, Quintel M, Herrmann P, et al. Airway pressure-time curve profile (stress index) detects tidal recruitment/hyperinflation in experimental acute lung injury. Crit Care Med. 2004;32(4):1018–27.
Ranieri VM, Giuliani R, Fiore T, Dambrosio M, Milic-Emili J. Volume-pressure curve of the respiratory system predicts effects of PEEP in ARDS: “occlusion” versus “constant flow” technique. Am J Resp Crit Care. 2012;149(1):19–27.
Grasso S, Stripoli T, Michele MD, Bruno F, Moschetta M, Angelelli G, et al. ARDSnet Ventilatory Protocol and Alveolar Hyperinflation. Am J Resp Crit Care. 2007;176(8):761–7.
Terragni PP, Filippini C, Slutsky AS, Birocco A, Tenaglia T, Grasso S, et al. Accuracy of plateau pressure and stress index to identify injurious ventilation in patients with acute respiratory distress syndrome. Anesthesiology. 2013;119(4):880–9.
Ranieri VM, Zhang H, Mascia L, Aubin M, Lin CY, Mullen JB, et al. Pressure–time curve predicts minimally injurious ventilatory strategy in an isolated rat lung model. Anesthesiology. 2000;93(5):1320–8.
Suter PM, Fairley HB, Isenberg MD. Optimum end-expiratory airway pressure in patients with acute pulmonary failure. NEJM. 1975;292(6):284–9.
Coffey RL, Albert RK, Robertson HT. Mechanisms of physiological dead space response to PEEP after acute oleic acid lung injury. J Appl Physiol. 1983;55(5):1550–7.
Fengmei G, Jin C, Songqiao L, Congshan Y, Yi Y. Dead space fraction changes during PEEP titration following lung recruitment in patients with ARDS. Respir Care. 2012;57(10):1578–85.
Maisch S, Reissmann H, Fuellekrug B, Weismann D, Rutkowski T, Tusman G, et al. Compliance and dead space fraction indicate an optimal level of positive end-expiratory pressure after recruitment in anesthetized patients. Anesth Analg. 2008;106(1):175–81.
Bonifazi M, Romitti F, Busana M, Palumbo MM, Steinberg I, Gattarello S, et al. End-tidal to arterial PCO2 ratio: a bedside meter of the overall gas exchanger performance. Intensive Care Med Exp. 2021;9(1):21.
Kallet RH, Lipnick MS. End-tidal-to-arterial pco2 ratio as signifier for physiologic dead-space ratio and oxygenation dysfunction in acute respiratory distress syndrome. Respir Care. 2020;66(2):263-8.
Sinha P, Fauvel NJ, Singh S, Soni N. Ventilatory ratio: a simple bedside measure of ventilation. BJA. 2009;102(5):692–7.
Sinha P, Fauvel NJ, Singh P, Soni N. Analysis of ventilatory ratio as a novel method to monitor ventilatory adequacy at the bedside. Crit Care. 2013;17(1):R34–R34.
Nuckton TJ, Alonso JA, Kallet RH, Daniel BM, Pittet JF, Eisner MD, et al. Pulmonary dead-space fraction as a risk factor for death in the acute respiratory distress syndrome. NEJM. 2002;346(17):1281–6.
Morales-Quinteros L, Schultz MJ, Bringué J, Calfee CS, Camprubí M, Cremer OL, et al. Estimated dead space fraction and the ventilatory ratio are associated with mortality in early ARDS. Ann Intensive Care. 2019;9(1):128.
Pintado MC, de Pablo R, Trascasa M, Milicua JM, Rogero S, Daguerre M, et al. Individualized PEEP setting in subjects with ARDS: a randomized controlled pilot study. Respir Care. 2013;58(9):1416–23.
Pintado MC, de Pablo R, Trascasa M, Milicua JM, Sánchez-García M. Compliance-guided versus FiO2-driven positive-end expiratory pressure in patients with moderate or severe acute respiratory distress syndrome according to the Berlin definition. Med Intensiva. 2017;41(5):277–84.
SuarezSipmann F, Böhm SH, Tusman G, Pesch T, Thamm O, Reissmann H, et al. Use of dynamic compliance for open lung positive end-expiratory pressure titration in an experimental study. Crit Care Med. 2007;35(1):214–21.
Levy P, Similowski T, Corbeil C, Albala M, Pariente R, Milic-Emili J, et al. A method for studying the static volume-pressure curves of the respiratory system during mechanical ventilation. J Crit Care. 1989;4(2):83–9.
Guttmann J, Eberhard L, Wolff G, Bertschmann W, Zeravik J, Adolph M. Maneuver-free determination of compliance and resistance in ventilated ARDS patients. Chest. 1992;102(4):1235–42.
Iotti GA, Braschi A, Brunner JX, Smits T, Olivei M, Palo A, et al. Respiratory mechanics by least squares fitting in mechanically ventilated patients: Applications during paralysis and during pressure support ventilation. Intensive Care Med. 1995;21(5):406–13.
Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. NEJM. 2015;372(8):747–55.
Williams EC, Motta-Ribeiro GC, Vidal Melo MF. Driving pressure and transpulmonary pressure. Anesthesiology. 2019;131(1):155–63.
Rezoagli E, Bellani G. How I set up positive end-expiratory pressure: evidence- and physiology-based! Crit Care. 2019;23(1):412.
Chen L, Sorbo LD, Grieco DL, Junhasavasdikul D, Rittayamai N, Soliman I, et al. Potential for lung recruitment estimated by the recruitment-to-inflation ratio in acute respiratory distress syndrome. A clinical trial. Am J Resp Crit Care. 2019;201(2):178–87.
Beloncle FM, Pavlovsky B, Desprez C, Fage N, Olivier PY, Asfar P, et al. Recruitability and effect of PEEP in SARS-Cov-2-associated acute respiratory distress syndrome. Ann Intensive Care. 2020;10(1):55.
Cour M, Biscarrat C, Stevic N, Degivry F, Argaud L, Guérin C. Recruitment-to-inflation ratio measured with modern intensive care unit ventilators: How accurate is it? Crit Care. 2022;26(1):85.
Cove ME, Pinsky MR, Marini JJ. PEEP, p-values, and pulmonary mechanics; don’t throw the baby out with the bathwater. Crit Care. 2022;26(1):309.
Rouby JJ, Puybasset L, Nieszkowska A, Lu Q. Acute respiratory distress syndrome: Lessons from computed tomography of the whole lung. Crit Care Med. 2003;31(4):S285–95.
Gattinoni L, Caironi P, Valenza F, Carlesso E. The role of CT-scan studies for the diagnosis and therapy of acute respiratory distress syndrome. Clin Chest Med. 2006;27(4):559–70.
Costamagna A, Pivetta E, Goffi A, Steinberg I, Arina P, Mazzeo AT, et al. Clinical performance of lung ultrasound in predicting ARDS morphology. Ann Intensive Care. 2021;11(1):51.
Bouhemad B, Brisson H, Le-Guen M, Arbelot C, Lu Q, Rouby JJ. Bedside ultrasound assessment of positive end-expiratory pressure–induced lung recruitment. Am J Resp Crit Care. 2011;183(3):341–7.
Mongodi S, Bouhemad B, Orlando A, Stella A, Tavazzi G, Via G, et al. Modified lung ultrasound score for assessing and monitoring pulmonary aeration. Ultraschall Med. 2017;38(05):530–7.
Mojoli F, Bouhemad B, Mongodi S, Lichtenstein D. Lung ultrasound for critically ill patients. Am J Resp Crit Care. 2018;199(6):701–14.
Longobardi S, Gaboardi P, Nava F, Lanza A, Rovere L, Ciceri L, et al. Lung ultrasound versus SpO2-guided as ‘best-PEEP’ titration in SARS-CoV2 ARDS. Eur Respir J. 2022;60:3850.
Costa EL, Borges JB, Melo A, Suarez-Sipmann F, Toufen C, Bohm SH, et al. Bedside estimation of recruitable alveolar collapse and hyperdistension by electrical impedance tomography. Intensive Care Med. 2009;35(6):1132–7.
Frerichs I, Amato MB, Van Kaam AH, Tingay DG, Zhao Z, Grychtol B, et al. Chest electrical impedance tomography examination, data analysis, terminology, clinical use and recommendations: consensus statement of the TRanslational EIT developmeNt stuDy group. Thorax. 2017;72(1):83.
Eronia N, Mauri T, Maffezzini E, Gatti S, Bronco A, Alban L, et al. Bedside selection of positive end-expiratory pressure by electrical impedance tomography in hypoxemic patients: a feasibility study. Ann Intensive Care. 2017;7(1):76.
Zhao Z, Chang MY, Chang MY, Gow CH, Zhang JH, Hsu YL, et al. Positive end-expiratory pressure titration with electrical impedance tomography and pressure–volume curve in severe acute respiratory distress syndrome. Ann Intensive Care. 2019;9(1):7.
He H, Chi Y, Yang Y, Yuan S, Long Y, Zhao P, et al. Early individualized positive end-expiratory pressure guided by electrical impedance tomography in acute respiratory distress syndrome: a randomized controlled clinical trial. Crit Care. 2021;25(1):230.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




