Right ventricular failure due to acute pulmonary embolism associated with Graves’ disease: A case report
Right ventricular failure associated with Graves’ disease
DOI:
https://doi.org/10.54205/ccc.v31.263457Keywords:
Acute pulmonary embolism, Graves’ disease, Right ventricular failureAbstract
Background
Graves' disease is a prevalent endocrine disorder characterized by diverse clinical manifestations affecting multiple organs, exhibiting varying degrees of severity. Cardiovascular system involvement is one of the most common manifestations, which include palpitation, tachycardia, cardiomyopathy, atrial fibrillation, pulmonary hypertension, or heart failure. Additionally, excessive thyroid hormone can lead to a hypercoagulable state, increasing the risk of venous thrombosis. However, thrombotic events, particularly deep vein thrombosis, cerebral venous thrombosis, or pulmonary embolism, are rare complications of Graves’ disease.
Case presentation
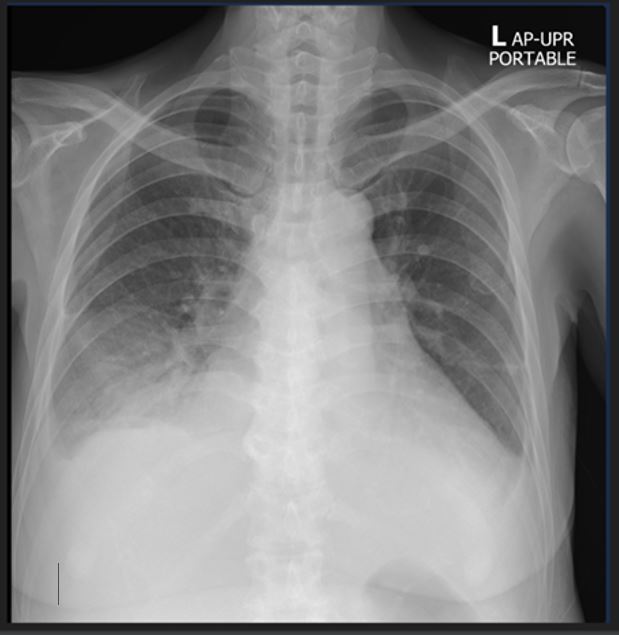
In this report, we present the case of a 53 years old woman who presented with progressively worsening dyspnea, orthopnea, paroxysmal nocturnal dyspnea, bilateral leg edema, and jaundice for 2 weeks. She had also reported a weight loss of 4 kilograms within 3 months. Upon admission to our hospital, she initially received a diagnosis of congestive heart failure with atrial fibrillation and thyrotoxicosis. Following diuretic therapy, the patient developed hypotension and severe hypoxemia. Subsequent investigation revealed acute right ventricular failure due to an acute sub-segmental pulmonary embolism, which was confirmed by computed tomography of the pulmonary artery. The patient's condition improved after resuscitation involving intravenous fluid administration to increase right ventricular preload, intravenous vasopressor infusion to elevate systemic blood pressure, management of severe thyrotoxicosis, and intravenous administration of heparin.
Conclusion
Graves’ disease, accompanied by hemodynamic disturbances due to acute right ventricular failure, necessitates admission to the intensive care unit for resuscitation and close monitoring. Although acute pulmonary embolism is an uncommon condition associated with Graves’ disease, it should be considered, particularly in patients who develop acute right ventricular failure.
Downloads
References
Lin HC, Yang LY, Kang JH. Increased risk of pulmonary embolism among patients with hyperthyroidism: a 5-year follow-up study. J Thromb Haemost. 2010;8(10):2176-81.
Kravets I. Hyperthyroidism: diagnosis and treatment. Am Fam Physician. 2016;93(5):363-70.
Biondi B, Kahaly GJ. Cardiovascular involvement in patients with different causes of hyperthyroidism. Nat Rev Endocrinol. 2010;6(8):431-43.
Satoh T, Isozaki O, Suzuki A, et al. 2016 Guidelines for the management of thyroid storm from the Japan thyroid association and Japan endocrine society (First edition). Endocr J. 2016;63(12):1025-1064.
Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. 2023;61(1).
Sugiura T, Yamanaka S, Takeuchi H, et al. Autoimmunity and pulmonary hypertension in patients with Graves’ disease. Heart and Vessels. 2015;30(5):642-646.
Araruna LVM, de Oliveira D, Pereira MC, et al. Interplay between thyroid hormone status and pulmonary hypertension in Graves’ disease: relevance of the assessment in thyrotoxic and Euthyroid patients. Frontiers in Endocrinology. 2022;12.
Zuhur SS, Baykiz D, Kara SP, et al. Relationship among pulmonary hypertension, autoimmunity, thyroid hormones and dyspnea in patients with hyperthyroidism. Am J Med Sci. 2017;353(4):374-380.
Grine S, Charfi N, Kamoun M, et al. Hyperthyroidism: A rare cause of pulmonary embolism: Report of two cases. Indian J Endocrinol Metab. 2013;17(6):1104-7.
Bisural R, Acharya D, Adhikari S, et al. Unprovoked isolated pulmonary embolism and Graves' disease in a patient with dyspnea: A case report. Cureus. 2022;14(5):e24972.
Lashari B, Qamar Z, Ahsan I, et al. Pulmonary embolism and hyperthyroidism: A rare association. Chest. 2016;150(4, Supplement):1213A.
Ali A, Mostafa W, Fernandez C, et al. Apathetic Thyroid storm with cardiorespiratory failure, pulmonary embolism, and coagulopathy in a young male with Graves' disease and myopathy. Case Rep Endocrinol. 2020;2020:8896777.
S. Y. Tang, S. H. Peng, C. H. Lin. J. K. Lee, S. C. Chou, and J. Y. Lu. Uncommon presentation of combined Graves’ disease and pulmonary embolism in a 32-year-old woman. Case report. Journal of internal medicine. 2019;30:351-357
Pussadhamma B. Acute pulmonary embolism. Srinagarind Med J. 2014;29(5):485-96.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




