Practical points of hemoperfusion in the intensive care unit
Hemoperfusion in critically ill patients
DOI:
https://doi.org/10.54205/ccc.v31.263679Keywords:
Blood purification, Hemoperfusion , Severe COVID-19, Acute respiratory distress syndromeAbstract
In cases of critical illness, some patients may experience adverse outcomes due to the excessive release of mediators or exposure to various toxins. These conditions can potentially lead to multi-organ failure and, ultimately, death. Hemoperfusion has emerged as an increasingly utilized method for blood purification, involving the removal of solutes by binding them to adsorbent materials. Currently, this technique is being employed in intensive care units to effectively clear many of the mediators and improve these critical conditions.
Hemoperfusion has demonstrated promising results in various conditions, including sepsis, severe Acute Respiratory Distress Syndrome (ARDS), acute liver failure, and severe Coronavirus Disease 2019 (COVID-19). Nonetheless, ongoing trials investigating various hemoperfusion techniques have yielded mixed results, necessitating further confirmation through additional studies.
Drawing upon my clinical experience and existing evidence, I advocate for a more personalized approach to initiating hemoperfusion therapy. I recommend evaluating each case individually and tailoring the treatment to optimize outcomes.
Downloads
References
Chakraborty RK, Burns B. Systemic inflammatory response syndrome. In:StatPearls. StatPearls Publishing; 2022. Accessed March 7, 2022. Available from: http://www.ncbi.nlm.nih.gov/books/NBK54 7669/
Ricci Z, Romagnoli S, Reis T, Bellomo R, Ronco C. Hemoperfusion in the intensive care unit. Intensive Care Med. 2022;48(10):1397-1408.
Ronco C, Bellomo R. Hemoperfusion: technical aspects and state of the art. Crit Care. 2022;26(1):135.
Ronco C, Chawla L, Husain-Syed F, Kellum J.A. Rationale for sequential extracorporeal therapy (SET) in sepsis. Critical Care. 2023,27:50
Sanfilippo F, Martucci G, Via LL, Cuttone G, Dimarco C, Arcadipane A, Astuto M. Hemoperfusion and blood purification strategies in patients with COVID-19: A systematic review. Artificial Organs. 2021;45:1466–76.
Datzmann T, Trager K. Extracorporeal membrane oxygenation and cytokine adsorption. J Thorac Dis. 2018,10:S653-S660
Surasit K, Srisawat N. The Efficacy of Early Additional Hemoperfusion Therapy for Severe COVID-19 Patients: A Prospective Cohort Study. Blood Purif. 2022;51(11):879-888.
Ronco C, Ricci Z, Husain-Syed F. From Multiple Organ Support Therapy to Extracorporeal Organ Support in Critically Ill Patients. Blood Purif. 2019;48(2): 99-105.
De Vriese AS, Colardyn FA, Philippé JJ, Vanholder RC, De Sutter JH, Lameire NH. Cytokine removal during continuous hemofiltration in septic patients. J Am Soc Nephrol. 1999;10(4):846–53.
Clark WR, Ferrari F, La Manna G, Ronco C. Extracorporeal sorbent technologies: basic concepts and clinical application. Contrib Nephrol. 2017;190:43–57.
Jung J, Eo E, Ahn KO. A case of hemoperfusion and L-carnitine management in valproic acid overdose. Am J Emerg Med. 2008;26(3):388.e3-4.
Baylis S, Costa-Pinto R, Hodgson S, Bellomo R, Baldwin I. Combined Hemoperfusion and Continuous Veno-Venous Hemofiltration for Carbamazepine Intoxication. Blood Purif. 2022;51(9):721-5.
Liu S, Xu L, Ma J, et al. High-volume continuous venovenous hemodiafiltration plus resin hemoperfusion improves severe metformin-associated toxicity. J Diabetes Investig. 2018;9(4):975-8.
Xiao Q, Wang W, Qi H, et al. Continuous hemoperfusion relieves pulmonary fibrosis in patients with acute mild and moderate paraquat poisoning. J Toxicol Sci. 2020;45(10):611-7.
Bo L. Therapeutic efficacies of different hemoperfusion frequencies in patients with organophosphate poisoning. Eur Rev Med Pharmacol Sci. 2014;18(22):3521–3.
Li Y, Qiu Z, Huang L, Cao C. Extracorporeal membrane oxygenation combined with sequential blood purification in the treatment of myocardial damage and cardiac arrest caused by mushroom poisoning. Toxicon. 2021;197:65–9.
Ghannoum M, Bouchard J, Nolin TD, Ouellet G, Roberts DM. Hemoperfusion for the treatment of poisoning: technology, determinant of poison clearance, and application in clinical practice. Seminars Dial. 2014;27:350–61.
Breuer T G K, Quast D R, Wiciok S, Ellrichmann G. Successful Treatment of Severe Digitoxin Intoxication with CytoSorb® Hemoadsorption. Blood Purif. 2021; 50 (1): 137–140.
Sazonov V, Tobylbayeva Z, Saparov A et al. New Therapeutic Approach to Reduce Methotrexate Toxicity after High-Dose Chemotherapy in a Child with Acute Lymphocytic Leukemia: Efficacy and Safety of Hemoadsorption with HA-230 Adsorber. Blood Purif. 2022;51(1):91-95.
Ma L, Zhang X, Ma W, Ding X. Meta-Analysis of the efficacy of DPMAS-based artificial liver in the treatment of ACLF. Research Square; 2022. [Epub]. DOI: 10.21203/rs.3.rs-1604197/v1.
Kittanamongkolchai W, El-Zoghby ZM, Eileen Hay J, et al. Charcoal hemoperfusion in the treatment of medically refractory pruritus in cholestatic liver disease. Hepatol Int. 2017;11(4):384–9.
Rittirsch D, Flierl MA, Ward PA. Harmful molecular mechanisms in sepsis. Nat Rev Immunol. 2008;8(10):776–87.
Seffer MT, Cottam D, Forni LG, Kielstein JT. Heparin 2.0: a new approach to the infection crisis. Blood Purif. 2021;50(1):28–34.
Ebeyer-Masotta M, Eichhorn T, Krajcik Laukova L, Weber V. ESAO 2021: adsorption of histones/nucleosomes, high-mobility group BOX-1 protein and platelet factor 4 by heparin-immobilized matrices (abstract). Int J Artif Organs. 2021;44:628–9.
Klein DJ, Foster D, Walker PM, Bagshaw SM, Mekonnen H, Antonelli M. Polymyxin B hemoperfusion in endotoxemic septic shock patients without extreme endotoxemia: a post hoc analysis of the EUPHRATES trial. Intensive Care Med. 2018;44(12):2205-12.
Schadler D, Pausch C, Heise D, Meier-Hellmann A, Brederlau J, Weiler N, Marx G, Putensen C, Spies C, Jorres A, et al. The effect of a novel extracorporeal cytokine hemoadsorption device on IL-6 elimination in septic patients: a randomized controlled trial. PLoS ONE. 2017;12(10): e0187015.
Huang Z, Wang SR, Yang ZL, Liu JY. Effect on extrapulmonary sepsis-induced acute lung injury by hemoperfusion with neutral microporous resin column. Ther Apher Dial. 2013;17(4):454-61.
Chu L, Li G, Yu Y, et al. Clinical effects of hemoperfusion combined with pulse high-volume hemofiltration on septic shock. Medicine. 2020;99: e19058
Broman ME, Hansson F, Vincent JL, Bodelsson M. Endotoxin and cytokine reducing properties of the oXiris membrane in patients with septic shock: A randomized crossover double-blind study. PLoS One. 2019;14(8):e0220444.
Xie J, Xiao W, Lin J. Effect of oXiris-CVVH on the Clinical Outcomes of Patients with Septic Shock: An Inverse Probability of Treatment-Weighted Analysis. Blood Purif. 2022;51(12):972-89.
Fajgenbaum DC, June CH. Cytokine storm. N Engl J Med. 2020;383:2255-73
Kim JS, Lee JY, Yang JW, et al. Immunopathogenesis and treatment of cytokine storm in COVID-19. Theranostics. 2021;11(1):316-29.
Nadim MK, Forni LG, Mehta RL, et al. COVID-19-associated acute kidney injury: consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup [published correction appears in Nat Rev Nephrol. 2020 Nov 2;:]. Nat Rev Nephrol. 2020;16(12):747-64.
Ruiz-Rodríguez JC, Plata-Menchaca EP, Chiscano-Camón L, Ruiz-Sanmartin A, Ferrer R. Blood purification in sepsis and COVID-19: what´s new in cytokine and endotoxin hemoadsorption. J Anesth Analg Crit Care. 2022;2(1):15.
Stockmann H, Thelen P, Stroben F, et al. CytoSorb Rescue for COVID-19 Patients With Vasoplegic Shock and Multiple Organ Failure: A Prospective, Open-Label, Randomized Controlled Pilot Study. Crit Care Med. 2022;50(6):964-76.
Supady A, Weber E, Rieder M, et al. Cytokine adsorption in patients with severe COVID-19 pneumonia requiring extracorporeal membrane oxygenation (CYCOV): a single centre, open-label, randomised, controlled trial. Lancet Respir Med. 2021;9(7):755-762.
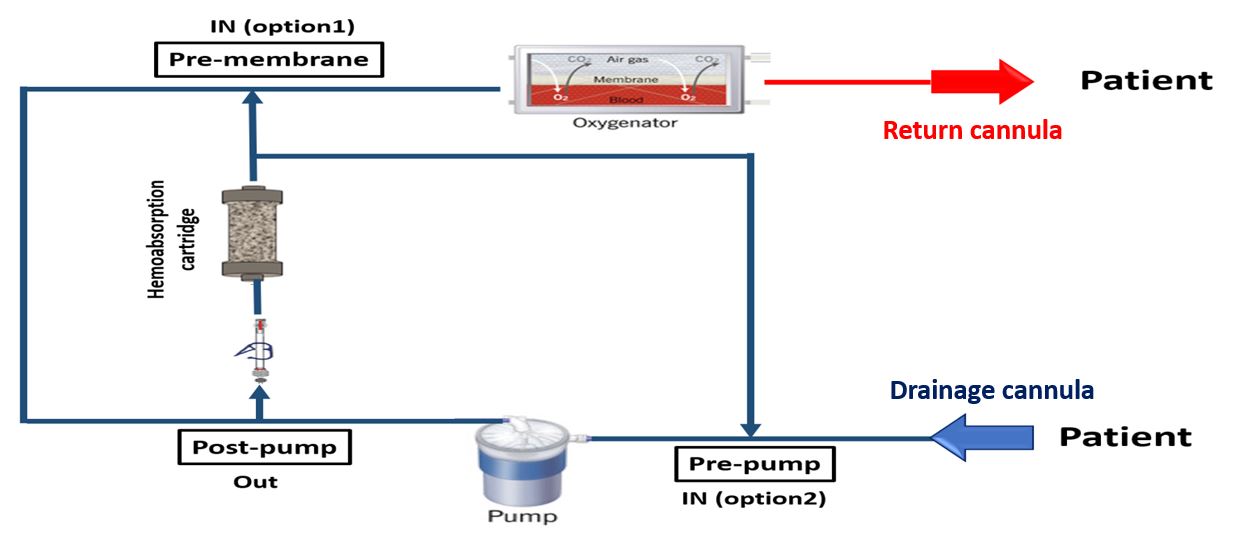
Napp LC, Ziegeler S, Kindgen-Milles D. Rationale of Hemoadsorption during Extracorporeal Membrane Oxygenation Support. Blood Purif. 2019;48(3):203-214.
Millar JE, Fanning JP, McDonald CI, McAuley DF, Fraser JF. The inflammatory response to extracorporeal membrane oxygenation (ECMO): a review of the pathophysiology. Crit Care. 2016;20(1):387.
Saetang P, Samransamruajkit R, Singjam K, Deekajorndech T. Polymyxin B Hemoperfusion in Pediatric Septic Shock: Single-Center Observational Case Series. Pediatr Crit Care Med. 2022;23(8):e386-e391.
Kielstein JT, Borchina DN, Fühner T, et al: Hemofiltration with the Seraph® 100 Microbind® affinity filter decreases SARSCoV-2 nucleocapsid protein in critically ill COVID-19 patients. Crit Care. 2021; 25:190
Chitty SA, Mobbs S, Rifkin BS, et al: A Multicenter Evaluation of the Seraph 100 Microbind Affinity Blood Filter for the Treatment of Severe COVID-19. Crit Care Explor. 2022;4(4):e0662.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




