Geo–economic variations in care for invasively ventilated patients: The potential benefits of closed–loop ventilation in resource–limited settings
Potential benefits of closed–loop ventilation in MIC
DOI:
https://doi.org/10.54205/ccc.v31.264920Keywords:
ICU, Critical care, Ventilation, Geo-economic variation, Closed-loop, Automated ventilationAbstract
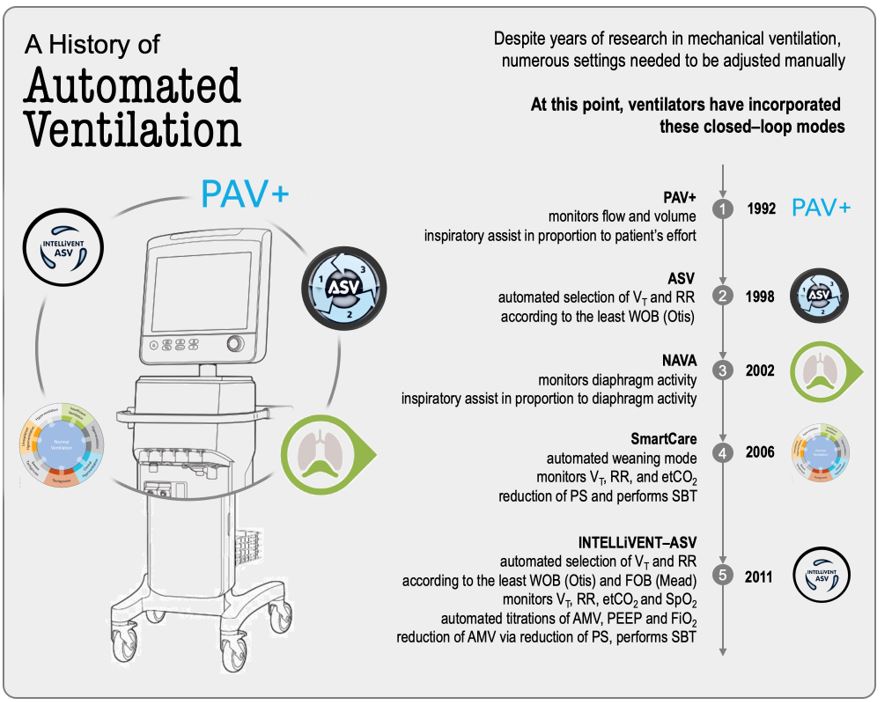
Lung–protective ventilation for invasively ventilated patients mimics normal breathing in which a low tidal volume is delivered at a specific respiratory rate with a limited inspiratory pressure on top of a sufficient level of positive end–expiratory pressure. It has been thoroughly demonstrated that despite being an expensive procedure, invasive ventilation when applied in a lung-protective way has a strong potential to improve the outcome of critically ill patients. However, implementing lung–protective ventilation has several challenges, including the fact that it can be quite time–consuming. One way to facilitate the use of lung–protective ventilation is to automate the settings involved with this strategy with closed–loop ventilation. In this review, we compare the epidemiology, ventilator management, and outcomes in critically ill ICU patients between middle–income countries and high–income countries and focus on the potentials and risks of closed–loop ventilation in middle–income countries.
Downloads
References
MacIntyre N, Rackley C, Khusid F. Fifty Years of Mechanical Ventilation-1970s to 2020. Crit Care Med. 2021;49(4):558-74.
Slutsky AS, Ranieri VM. Ventilator-Induced Lung Injury. New England Journal of Medicine. 2013;369(22):2126-36.
Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. Jama. 2016;315(8):788-800.
Buiteman-Kruizinga LA, Serpa Neto A, Schultz MJ. Automation to improve lung protection. Intensive Care Med. 2022;48(7):943-6.
Serpa Neto A, Checkley W, Sivakorn C, Hashmi M, Papali A, Schultz MJ. Pragmatic Recommendations for the Management of Acute Respiratory Failure and Mechanical Ventilation in Patients with COVID-19 in Low- and Middle-Income Countries. Am J Trop Med Hyg. 2021;104(3_Suppl):60-71.
Serpa Neto A, Schultz MJ, Festic E. Ventilatory support of patients with sepsis or septic shock in resource-limited settings. Intensive Care Med. 2016;42(1):100-3.
Hung TM, Van Hao N, Yen LM, McBride A, Dat VQ, van Doorn HR, et al. Direct Medical Costs of Tetanus, Dengue, and Sepsis Patients in an Intensive Care Unit in Vietnam. Front Public Health. 2022;10:893200.
Schultz MJ, Dunser MW, Dondorp AM, Adhikari NK, Iyer S, Kwizera A, et al. Current challenges in the management of sepsis in ICUs in resource-poor settings and suggestions for the future. Intensive Care Med. 2017;43(5):612-24.
Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301-8.
Botta M, Tsonas AM, Pillay J, Boers LS, Algera AG, Bos LDJ, et al. Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): a national, multicentre, observational cohort study. Lancet Respir Med. 2021;9(2):139-48.
Simonis FD, Serpa Neto A, Binnekade JM, Braber A, Bruin KCM, Determann RM, et al. Effect of a Low vs Intermediate Tidal Volume Strategy on Ventilator-Free Days in Intensive Care Unit Patients Without ARDS: A Randomized Clinical Trial. Jama. 2018;320(18):1872-80.
Helmerhorst HJ, Schultz MJ, van der Voort PH, de Jonge E, van Westerloo DJ. Bench-to-bedside review: the effects of hyperoxia during critical illness. Crit Care. 2015;19(1):284.
Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8):747-55.
Serpa Neto A, Deliberato RO, Johnson AEW, Bos LD, Amorim P, Pereira SM, et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44(11):1914-22.
van Meenen DMP, Algera, AGA, Schuijt, MTU, Simonis, FD, van der Hoeven, SM, Serpa Neto, A, Gama de Abreu, M, Pelosi, P, Paulus, F, Schultz, MJ. Effect of Mechanical Power on Mortality in Invasively Ventilated ICU patients without ARDS––An Individual Patient Data–analysis of Three Randomized Clinical Trials. European Journal of Anesthesiology. 2022; in press.
Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351(4):327-36.
Meade MO, Cook DJ, Guyatt GH, Slutsky AS, Arabi YM, Cooper DJ, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. Jama. 2008;299(6):637-45.
Mercat A, Richard JC, Vielle B, Jaber S, Osman D, Diehl JL, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. Jama. 2008;299(6):646-55.
Cavalcanti AB, Suzumura É A, Laranjeira LN, Paisani DM, Damiani LP, Guimarães HP, et al. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on Mortality in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. Jama. 2017;318(14):1335-45.
Briel M, Meade M, Mercat A, Brower RG, Talmor D, Walter SD, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. Jama. 2010;303(9):865-73.
Ball L, Serpa Neto A, Trifiletti V, Mandelli M, Firpo I, Robba C, et al. Effects of higher PEEP and recruitment manoeuvres on mortality in patients with ARDS: a systematic review, meta-analysis, meta-regression and trial sequential analysis of randomized controlled trials. Intensive Care Med Exp. 2020;8(Suppl 1):39.
Dianti J, Tisminetzky M, Ferreyro BL, Englesakis M, Del Sorbo L, Sud S, et al. Association of Positive End-Expiratory Pressure and Lung Recruitment Selection Strategies with Mortality in Acute Respiratory Distress Syndrome: A Systematic Review and Network Meta-analysis. Am J Respir Crit Care Med. 2022;205(11):1300-10.
Constantin JM, Jabaudon M, Lefrant JY, Jaber S, Quenot JP, Langeron O, et al. Personalised mechanical ventilation tailored to lung morphology versus low positive end-expiratory pressure for patients with acute respiratory distress syndrome in France (the LIVE study): a multicentre, single-blind, randomised controlled trial. Lancet Respir Med. 2019;7(10):870-80.
Pelosi P, Ball L, Barbas CSV, Bellomo R, Burns KEA, Einav S, et al. Personalized mechanical ventilation in acute respiratory distress syndrome. Crit Care. 2021;25(1):250.
Laffey JG, Bellani G, Pham T, Fan E, Madotto F, Bajwa EK, et al. Potentially modifiable factors contributing to outcome from acute respiratory distress syndrome: the LUNG SAFE study. Intensive Care Med. 2016;42(12):1865-76.
Algera AG, Pisani L, Serpa Neto A, den Boer SS, Bosch FFH, Bruin K, et al. Effect of a Lower vs Higher Positive End-Expiratory Pressure Strategy on Ventilator-Free Days in ICU Patients Without ARDS: A Randomized Clinical Trial. Jama. 2020;324(24):2509-20.
Urner M, Jüni P, Hansen B, Wettstein MS, Ferguson ND, Fan E. Time-varying intensity of mechanical ventilation and mortality in patients with acute respiratory failure: a registry-based, prospective cohort study. Lancet Respir Med. 2020;8(9):905-13.
Georgopoulos D, Xirouchaki N, Tzanakis N, Younes M. Data on respiratory variables in critically ill patients with acute respiratory failure placed on proportional assist ventilation with load adjustable gain factors (PAV+). Data Brief. 2016;8:484-93.
Burns KE, Lellouche F, Nisenbaum R, Lessard MR, Friedrich JO. Automated weaning and SBT systems versus non-automated weaning strategies for weaning time in invasively ventilated critically ill adults. Cochrane Database Syst Rev. 2014;2014(9):Cd008638.
Kampolis CF, Mermiri M, Mavrovounis G, Koutsoukou A, Loukeri AA, Pantazopoulos I. Comparison of advanced closed-loop ventilation modes with pressure support ventilation for weaning from mechanical ventilation in adults: A systematic review and meta-analysis. J Crit Care. 2021;68:1-9.
Botta M, Tsonas AM, Sinnige JS, De Bie AJR, Bindels A, Ball L, et al. Effect of Automated Closed-loop ventilation versus convenTional VEntilation on duration and quality of ventilation in critically ill patients (ACTiVE) - study protocol of a randomized clinical trial. Trials. 2022;23(1):348.
Lellouche F, Bouchard PA, Simard S, L'Her E, Wysocki M. Evaluation of fully automated ventilation: a randomized controlled study in post-cardiac surgery patients. Intensive Care Med. 2013;39(3):463-71.
Arnal JM, Saoli M, Garnero A. Airway and transpulmonary driving pressures and mechanical powers selected by INTELLiVENT-ASV in passive, mechanically ventilated ICU patients. Heart Lung. 2020;49(4):427-34.
De Bie AJR, Neto AS, van Meenen DM, Bouwman AR, Roos AN, Lameijer JR, et al. Fully automated postoperative ventilation in cardiac surgery patients: a randomised clinical trial. Br J Anaesth. 2020;125(5):739-49.
Wendel Garcia PD, Hofmaenner DA, Brugger SD, Acevedo CT, Bartussek J, Camen G, et al. Closed-Loop Versus Conventional Mechanical Ventilation in COVID-19 ARDS. J Intensive Care Med. 2021;36(10):1184-93.
Buiteman-Kruizinga LA, Mkadmi HE, Serpa Neto A, Kruizinga MD, Botta M, Schultz MJ, et al. Effect of INTELLiVENT-ASV versus Conventional Ventilation on Ventilation Intensity in Patients with COVID-19 ARDS-An Observational Study. J Clin Med. 2021;10(22).
Pisani L, Algera AG, Neto AS, Azevedo L, Pham T, Paulus F, et al. Geoeconomic variations in epidemiology, ventilation management, and outcomes in invasively ventilated intensive care unit patients without acute respiratory distress syndrome: a pooled analysis of four observational studies. Lancet Glob Health. 2022;10(2):e227-e35.
Laffey JG, Madotto F, Bellani G, Pham T, Fan E, Brochard L, et al. Geo-economic variations in epidemiology, patterns of care, and outcomes in patients with acute respiratory distress syndrome: insights from the LUNG SAFE prospective cohort study. Lancet Respir Med. 2017;5(8):627-38.
Pisani L, Algera AG, Serpa Neto A, Ahsan A, Beane A, Chittawatanarat K, et al. PRactice of VENTilation in Middle-Income Countries (PRoVENT-iMIC): rationale and protocol for a prospective international multicentre observational study in intensive care units in Asia. BMJ Open. 2018;8(4):e020841.
Pisani L, Algera AG, Serpa Neto A, Ahsan A, Beane A, Chittawatanarat K, et al. Epidemiological Characteristics, Ventilator Management, and Clinical Outcome in Patients Receiving Invasive Ventilation in Intensive Care Units from 10 Asian Middle-Income Countries (PRoVENT-iMiC): An International, Multicenter, Prospective Study. Am J Trop Med Hyg. 2021;104(3):1022-33.
Azevedo LC, Park M, Salluh JI, Rea-Neto A, Souza-Dantas VC, Varaschin P, et al. Clinical outcomes of patients requiring ventilatory support in Brazilian intensive care units: a multicenter, prospective, cohort study. Crit Care. 2013;17(2):R63.
Neto AS, Barbas CSV, Simonis FD, Artigas-Raventós A, Canet J, Determann RM, et al. Epidemiological characteristics, practice of ventilation, and clinical outcome in patients at risk of acute respiratory distress syndrome in intensive care units from 16 countries (PRoVENT): an international, multicentre, prospective study. Lancet Respir Med. 2016;4(11):882-93.
British Medical Association. Medical staffing in England: a defining moment for doctors and patients. London; 2021.
Angus DC, Kelley MA, Schmitz RJ, White A, Popovich J, Jr. Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? Jama. 2000;284(21):2762-70.
Bialais E, Wittebole X, Vignaux L, Roeseler J, Wysocki M, Meyer J, et al. Closed-loop ventilation mode (IntelliVent®-ASV) in intensive care unit: a randomized trial. Minerva Anestesiol. 2016;82(6):657-68.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




