Critical care echocardiography in shock: A comprehensive review
Critical care echocardiography in shock: A comprehensive review
DOI:
https://doi.org/10.54205/ccc.v31.265335Keywords:
Critical care echocardiography, Shock, Left ventricular function, Right ventricular function, Pericardial effusion, Preload responsivenessAbstract
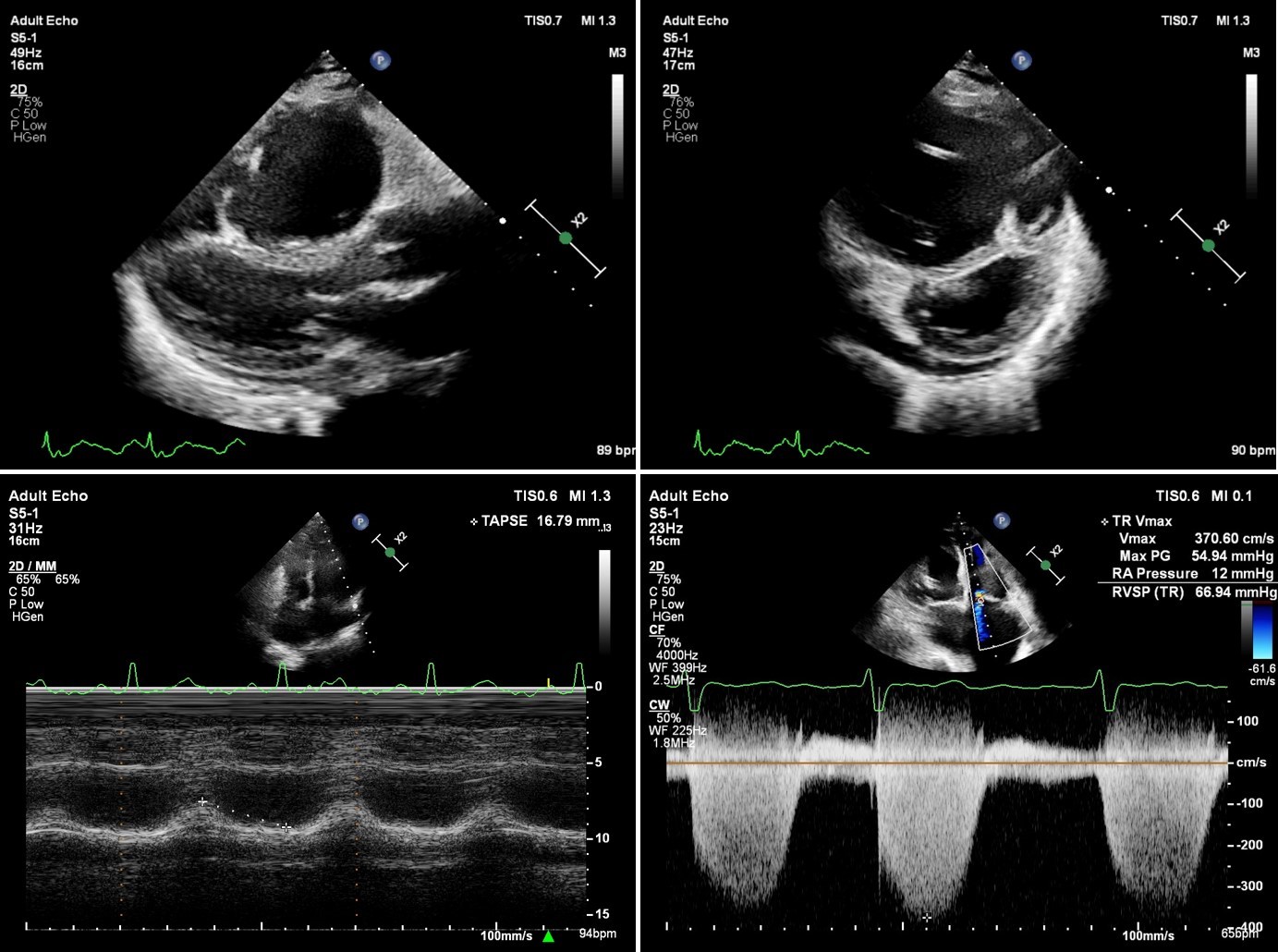
Bedside transthoracic echocardiography is a valuable tool for assessing cardiac morphology and function in critically ill patients. It provides real-time information and aids in making prompt clinical decisions. This article aims to explore the role of critical care echocardiography, especially during shock resuscitation, focusing on basic image acquisition and interpretation. The review discusses the evaluation of left ventricular function, right ventricular function, preload responsiveness, the presence of pericardial effusion, and tamponade.
Downloads
References
Díaz-Gómez JL, Mayo PH, Koenig SJ. Point-of-Care Ultrasonography. N Engl J Med. 2021;385(17):1593-1602.
Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013;369(18):1726-34.
Orme RM, Oram MP, McKinstry CE. Impact of echocardiography on patient management in the intensive care unit: an audit of district general hospital practice. Br J Anaesth. 2009;102(3):340-4.
Feng M, McSparron JI, Kien DT, Stone DJ, Roberts DH, Schwartzstein RM, Vieillard-Baron A, Celi LA. Transthoracic echocardiography and mortality in sepsis: analysis of the MIMIC-III database. Intensive Care Med. 2018;44(6):884-892.
Papolos A, Narula J, Bavishi C, Chaudhry FA, Sengupta PP. U.S. Hospital Use of Echocardiography: Insights From the Nationwide Inpatient Sample. J Am Coll Cardiol. 2016;67(5):502-11.
Yoshida T, Yoshida T, Noma H, Nomura T, Suzuki A, Mihara T. Diagnostic accuracy of point-of-care ultrasound for shock: a systematic review and meta-analysis. Crit Care. 2023;27(1):200.
Levitov A, Frankel HL, Blaivas M, et al. Guidelines for the Appropriate Use of Bedside General and Cardiac Ultrasonography in the Evaluation of Critically Ill Patients-Part II: Cardiac Ultrasonography. Crit Care Med. 2016;44(6):1206-27.
Via G, Hussain A, Wells M, et al. International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr. 2014;27(7):683.e1-683.e33.
Mitchell C, Rahko PS, Blauwet LA, et al. Guidelines for Performing a Comprehensive Transthoracic Echocardiographic Examination in Adults: Recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2019;32(1):1-64.
Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1-39.e14.
Paonessa JR, Brennan T, Pimentel M, Steinhaus D, Feng M, Celi LA. Hyperdynamic left ventricular ejection fraction in the intensive care unit. Crit Care. 2015;19(1):288.
Wehner GJ, Jing L, Haggerty CM, et al. Routinely reported ejection fraction and mortality in clinical practice: where does the nadir of risk lie? Eur Heart J. 2020;41(12):1249-1257.
Gudmundsson P, Rydberg E, Winter R, et al. Visually estimated left ventricular ejection fraction by echocardiography is closely correlated with formal quantitative methods. Int J Cardiol. 2005;101(2):209-212.
Orde S, Slama M, Hilton A, Yastrebov K, McLean A. Pearls and pitfalls in comprehensive critical care echocardiography. Crit Care. 2017;21(1):279.
Sanfilippo F, Scolletta S, Morelli A, et al. Practical approach to diastolic dysfunction in light of the new guidelines and clinical applications in the operating room and in the intensive care. Ann Intensive Care. 2018;8(1):100.
Lanspa MJ, Gutsche AR, Wilson EL, et al. Application of a simplified definition of diastolic function in severe sepsis and septic shock. Crit Care. 2016;20(1):243.
Mitter SS, Shah SJ, Thomas JD. A Test in Context: E/A and E/e' to Assess Diastolic Dysfunction and LV Filling Pressure. J Am Coll Cardiol. 2017;69:1451–1464.
Sharifov OF, Schiros CG, Aban I, et al. Diagnostic accuracy of tissue Doppler index E/e' for evaluating left ventricular filling pressure and diastolic dysfunction/heart failure with preserved ejection fraction: A systematic review and meta-analysis. J Am Heart Assoc. 2016;5(1):e002530.
Nagueh SF, Middleton KJ, Kopelen HA, et al. Doppler tissue imaging: A noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997;30(6):1527-1533.
Tongyoo S, Jakrapanichakul D, Chaowalit N. Estimation of left ventricular end-diastolic pressure by tissue Doppler imaging in patients with coronary artery disease. Thai Heart J. 2006;19(3):29–37.
Tongyoo S, Thomrongpairoj P, Permpikul C. Efficacy of echocardiography during spontaneous breathing trial with low-level pressure support for predicting weaning failure among medical critically ill patients. Echocardiography. 2019;36:659–665.
Thitayanapong A, Tongyoo S. Left ventricular diastolic functioncompared to inferiorvena cava diameter variation as predictor of fluidresponsiveness in mechanical ventilated patients with shock:Theresearch protocol. Clin Crit Care. 2022;30:e0010.
Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543-603.
Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: A report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685.
Tongyoo S, Sangnopakunsri W, Permpikul C. Transthoracic echocardiogram for the diagnosis of right ventricular dysfunction in critically ill patients. J Med Assoc Thai. 2014;97(suppl. 1):S84–S92.
Galiè N, Humbert M, Vachiery JL, et al.Echocardiographic Screening Methods for Pulmonary Hypertension: A Practical Review. J Cardiovasc Imaging. 2020;28(1):1-9.
McCanny P, Colreavy F. Echocardiographic approach to cardiac tamponade in critically ill patients. J Crit Care. 2017;39:271-277.
Alerhand S, Carter JM. What echocardiographic findings suggest a pericardial effusion is causing tamponade? Am J Emerg Med. 2019;37(2):321-326.
Mandeville JC, Colebourn CL. Can transthoracic echocardiography be used to predict fluid responsiveness in the critically ill patient? A systematic review. Crit Care Res Pract. 2012;2012:513480.
Blanco P. Rationale for Using the Velocity–Time Integral and the Minute Distance for Assessing the Stroke Volume and Cardiac Output in Point-of-Care Settings. Ultrasound J. 2020;12:21.
Franchi F, Vetrugno L, Scolletta S. Echocardiography to guide fluid therapy in critically ill patients: Check the heart and take a quick look at the lungs. J Thorac Dis. 2017;9(2):477-481.
Via G., Tavazzi G., Price S. Ten Situations Where Inferior Vena Cava Ultrasound May Fail to Accurately Predict Fluid Responsiveness: A Physiologically Based Point of View. Intensive Care Med. 2016;42:1164–1167.
Huang H, Shen Q, Liu Y, et al. Value of variation index of inferior vena cava diameter in predicting fluid responsiveness in patients with circulatory shock receiving mechanical ventilation: A systematic review and meta-analysis. Crit Care. 2018;22:204.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




