Sedation management in the post-COVID era: A personalised, patient-orientated approach
A personalised, patient-orientated approach to ICU sedation
DOI:
https://doi.org/10.54205/ccc.v32.265724Keywords:
Hypnotics and sedatives, Delirium, Critical illness, Mechanical ventilation, DexmedetomidineAbstract
Intensive care patients are older, frailer, and more co-morbid than ever before, and remain at risk of a variety of adverse outcomes, both in ICU, and after discharge. Sedation and delirium play an intricate role in this complex system, and it can be difficult to determine if they are a contributor or consequence in any given situation. During the COVID-19 pandemic, the increased frequency of complex ventilatory management, including prone ventilation and neuromuscular blockade, necessitated deep sedation in many cases. In concert with infection control concerns and staffing pressures, the delivery of precision symptom- and patient-oriented sedation has waned in favour of strategies felt to be globally safe. Using the SPICE III study as a lens to understand both the importance of exploring heterogeneity of effect in large, complex RCTs of critically ill patients, and the importance of an individualised approach to sedation in the intensive care unit, we demonstrate the evolution of our understanding of sedation in this challenging environment. By following the principles that define the cornerstones of best contemporary sedation practice we can once more grow beyond the boundaries of clinical practice guidelines in the provision of personalised, patient-orientated sedation in the post-COVID intensive care unit.
Downloads
References
Darvall JN, Bellomo R, Paul E, Subramaniam A, Santamaria JD, Bagshaw SM, et al. Frailty in very old critically ill patients in Australia and New Zealand: a population-based cohort study. The Medical Journal of Australia. 2019;211:318-23.
Sahle BW, Pilcher D, Litton E, Ofori-Asenso R, Peter K, McFadyen J, et al. Association between frailty, delirium, and mortality in older critically ill patients: a binational registry study. Annals of Intensive Care. 2022;12:108.
Rai S, Brace C, Ross P, Darvall J, Haines K, Mitchell I, et al. Characteristics and Outcomes of Very Elderly Patients Admitted to Intensive Care: A Retrospective Multicenter Cohort Analysis. Critical Care Medicine. 2023;51:1328-38.
Moran JL, Bristow P, Solomon PJ, George C, Hart GK, Australian, et al. Mortality and length-of-stay outcomes, 1993-2003, in the binational Australian and New Zealand intensive care adult patient database. Critical Care Medicine. 2008;36:46-61.
Laupland KB, Tabah A, Holley AD, Bellapart J, Pilcher DV. Decreasing Case-Fatality But Not Death Following Admission to ICUs in Australia, 2005-2018. Chest. 2021;159:1503-6.
Iwashyna TJ, Hodgson CL, Pilcher D, Bailey M, Bellomo R. Persistent critical illness characterised by Australian and New Zealand ICU clinicians. Critical Care and Resuscitation: Journal of the Australasian Academy of Critical Care Medicine. 2015;17:153-8.
Iwashyna TJ, Hodgson CL, Pilcher D, Bailey M, van Lint A, Chavan S, et al. Timing of onset and burden of persistent critical illness in Australia and New Zealand: a retrospective, population-based, observational study. The Lancet. Respiratory Medicine. 2016;4:566-73.
Shaw M, Viglianti EM, McPeake J, Bagshaw SM, Pilcher D, Bellomo R, et al. Timing of Onset, Burden, and Postdischarge Mortality of Persistent Critical Illness in Scotland, 2005-2014: A Retrospective, Population-Based, Observational Study. Critical Care. Explorations 2020;2:e0102.
Hammond NE, Finfer SR, Li Q, Taylor C, Cohen J, Arabi Y, et al. Health-related quality of life in survivors of septic shock: 6-month follow-up from the ADRENAL trial. Intensive Care Medicine. 2020;46:1696-706.
Bulic D, Bennett M, Georgousopoulou EN, Shehabi Y, Pham T, Looi JCL, et al. Cognitive and psychosocial outcomes of mechanically ventilated intensive care patients with and without delirium. Annals of Intensive Care. 2020;10:104.
Ladha KS, Cuthbertson BH, Abbott TEF, Pearse RM, Wijeysundera DN. Functional decline after major elective non-cardiac surgery: a multicentre prospective cohort study. Anaesthesia. 2021;76:1593-9.
Gallagher M, Cass A, Bellomo R, Finfer S, Gattas D, Lee J, et al. Long-Term Survival and Dialysis Dependency Following Acute Kidney Injury in Intensive Care: Extended Follow-up of a Randomized Controlled Trial. PLoS Medicine. 2014;11:e1001601.
See EJ, Jayasinghe K, Glassford N, Bailey M, Johnson DW, Polkinghorne KR, et al. Long-term risk of adverse outcomes after acute kidney injury: a systematic review and meta-analysis of cohort studies using consensus definitions of exposure. Kidney International. 2019;95:160-72.
Goldberg TE, Chen C, Wang Y, Jung E, Swanson A, Ing C, et al. Association of Delirium With Long-term Cognitive Decline: A Meta-analysis. JAMA Neurology. 2020;77:1373.
Fong TG, Inouye SK. The inter-relationship between delirium and dementia: the importance of delirium prevention. Nature Reviews Neurology. 2022;18:579-96.
Doherty Z, Kippen R, Bevan D, Duke G, Williams S, Wilson A, et al. Long-term outcomes of hospital survivors following an ICU stay: A multi-centre retrospective cohort study. PloS One. 2022;17:e0266038.
Florescu S, Stanciu D, Zaharia M, Kosa A, Codreanu D, Kidwai A, et al. Long-term (180-Day) Outcomes in Critically Ill Patients With COVID-19 in the REMAP-CAP Randomized Clinical Trial. JAMA. 2023;329:39.
Shehabi Y, Al-Bassam W, Pakavakis A, Murfin B, Howe B. Optimal Sedation and Pain Management: A Patient- and Symptom-Oriented Paradigm. Seminars in Respiratory and Critical Care Medicine. 2021;42:098-111.
Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJC, Pandharipande PP, et al. Executive Summary: Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Critical Care Medicine. 2018;46:1532-48.
Ward DS, Absalom AR, Aitken LM, Balas MC, Brown DL, Burry L, et al. Design of Clinical Trials Evaluating Sedation in Critically Ill Adults Undergoing Mechanical Ventilation: Recommendations From Sedation Consortium on Endpoints and Procedures for Treatment, Education, and Research (SCEPTER) Recommendation III. Critical Care Medicine. 2021;49:1684-93.
Luz M, Brandão Barreto B, De Castro REV, Salluh J, Dal-Pizzol F, Araujo C, et al. Practices in sedation, analgesia, mobilization, delirium, and sleep deprivation in adult intensive care units (SAMDS-ICU): an international survey before and during the COVID-19 pandemic. Annals of Intensive Care. 2022;12:9.
Saberon KMQ, Rosario Soliven J-A. The Association of Proning and Stroke among Deeply Sedated Critically Ill SARS-CoV-2 (COVID-19) Patients. Neurology Research International. 2022;2022:6348888.
Rasulo FA, Badenes R, Longhitano Y, Racca F, Zanza C, Marchesi M, et al. Excessive Sedation as a Risk Factor for Delirium: A Comparison between Two Cohorts of ARDS Critically Ill Patients with and without COVID-19. Life (Basel, Switzerland). 2022;12:2031.
Machado-Duque ME, Gaviria-Mendoza A, Valladales-Restrepo LF, Albanés-Beltrán JP, Machado-Alba JE. Trends in the Use of Sedative-Hypnotics, Opioids, and Neuromuscular Blockers in Hospitalized Patients During the COVID-19 Pandemic: Observational Retrospective Study. Drugs - Real World Outcomes. 2022;9:629-38.
Stephens RJ, Evans EM, Pajor MJ, Pappal RD, Egan HM, Wei M, et al. A dual-center cohort study on the association between early deep sedation and clinical outcomes in mechanically ventilated patients during the COVID-19 pandemic: The COVID-SED study. Critical Care (London, England). 2022;26:179.
Liu K, Nakamura K, Katsukawa H, Nydahl P, Ely EW, Kudchadkar SR, et al. Implementation of the ABCDEF Bundle for Critically Ill ICU Patients During the COVID-19 Pandemic: A Multi-National 1-Day Point Prevalence Study. Frontiers in Medicine. 2021;8:735860.
Liu K, Nakamura K, Katsukawa H, Elhadi M, Nydahl P, Ely EW, et al. ABCDEF Bundle and Supportive ICU Practices for Patients With Coronavirus Disease 2019 Infection: An International Point Prevalence Study. Critical Care Explorations. 2021;3:e0353.
Kwon S, Kim M, Choi S. Ethical dilemmas and care actions in nurses providing palliative sedation. Nursing Ethics. 2022;29:1220-30.
Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Critical Care Medicine. 2013;41:263-306.
Pandharipande PP, Pun BT, Herr DL, Maze M, Girard TD, Miller RR, et al. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA. 2007;298:2644-53.
Muller L, Chanques G, Bourgaux C, Louart G, Jaber S, Fabbro-Peray P, et al. Impact of the use of propofol remifentanil goal-directed sedation adapted by nurses on the time to extubation in mechanically ventilated ICU patients: the experience of a French ICU. Annales Francaises D'anesthesie Et De Reanimation. 2008;27:481.e1-8.
Samuelson KaM, Lundberg D, Fridlund B. Light vs. heavy sedation during mechanical ventilation after oesophagectomy--a pilot experimental study focusing on memory. Acta Anaesthesiologica Scandinavica. 2008;52:1116-23.
Treggiari MM, Romand J-A, Yanez ND, Deem SA, Goldberg J, Hudson L, et al. Randomized trial of light versus deep sedation on mental health after critical illness. Critical Care Medicine. 2009;37:2527-34.
Strøm T, Martinussen T, Toft P. A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomised trial. Lancet (London, England). 2010;375:475-80.
Shehabi Y, Bellomo R, Reade MC, Bailey M, Bass F, Howe B, et al. Early goal-directed sedation versus standard sedation in mechanically ventilated critically ill patients: a pilot study*. Critical Care Medicine. 2013;41:1983-91.
Bugedo G, Tobar E, Aguirre M, Gonzalez H, Godoy J, Lira MT, et al. The implementation of an analgesia-based sedation protocol reduced deep sedation and proved to be safe and feasible in patients on mechanical ventilation. Revista Brasileira De Terapia Intensiva. 2013;25:188-96.
Tanaka LMS, Azevedo LCP, Park M, Schettino G, Nassar AP, Réa-Neto A, et al. Early sedation and clinical outcomes of mechanically ventilated patients: a prospective multicenter cohort study. Critical Care (London, England). 2014;18:R156.
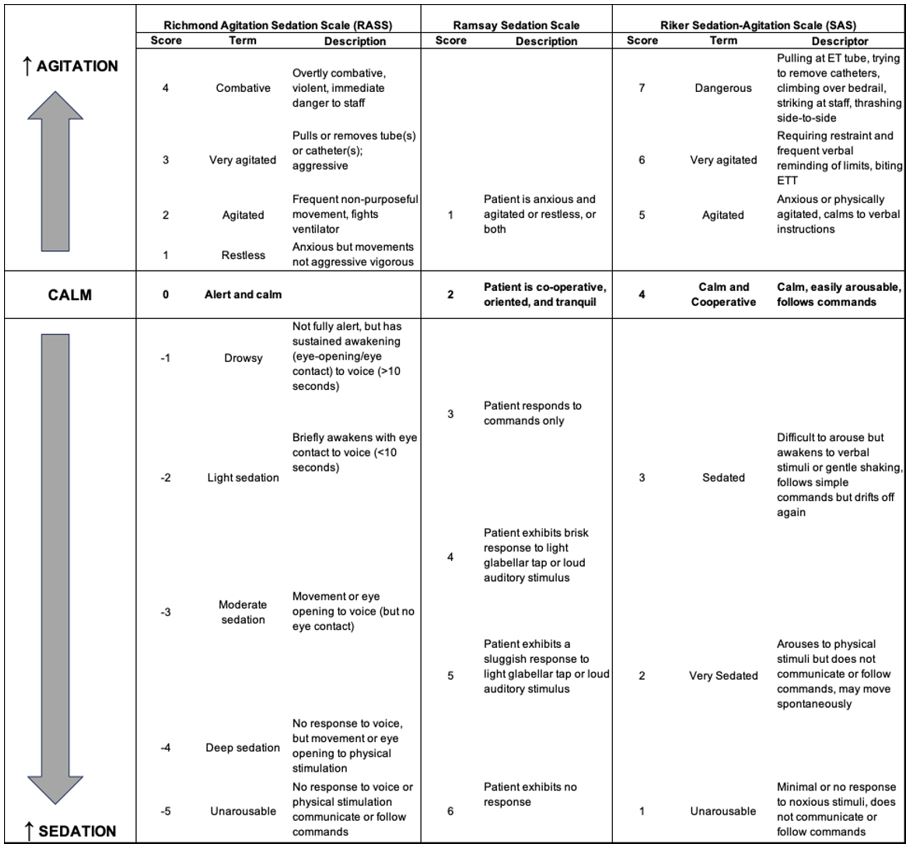
Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. American Journal of Respiratory and Critical Care Medicine. 2002;166:1338-44.
Khan BA, Guzman O, Campbell NL, Walroth T, Tricker JL, Hui SL, et al. Comparison and Agreement Between the Richmond Agitation-Sedation Scale and the Riker Sedation-Agitation Scale in Evaluating Patients' Eligibility for Delirium Assessment in the ICU. Chest. 2012;142:48-54.
Riessen R, Pech R, Tränkle P, Blumenstock G, Haap M. Comparison of the RAMSAY score and the Richmond Agitation Sedation Score for the measurement of sedation depth. Critical Care. 2012;16:P326,-cc10933.
Shehabi Y, Bellomo R, Kadiman S, Ti LK, Howe B, Reade MC, et al. Sedation Intensity in the First 48 Hours of Mechanical Ventilation and 180-Day Mortality: A Multinational Prospective Longitudinal Cohort Study*. Critical Care Medicine. 2018;46:850-9.
Stephens RJ, Dettmer MR, Roberts BW, Ablordeppey E, Fowler SA, Kollef MH, et al. Practice Patterns and Outcomes Associated With Early Sedation Depth in Mechanically Ventilated Patients: A Systematic Review and Meta-Analysis. Critical Care Medicine. 2018;46:471-9.
Nassar AP, Zampieri FG, Salluh JI, Bozza FA, Machado FR, Guimarães HP, et al. Organizational factors associated with target sedation on the first 48 h of mechanical ventilation: an analysis of checklist-ICU database. Critical Care (London, England). 2019;23:34.
Cavalcanti AB, Bozza FA, Machado FR, Salluh JIF, Campagnucci VP, Vendramim P, et al. Effect of a Quality Improvement Intervention With Daily Round Checklists, Goal Setting, and Clinician Prompting on Mortality of Critically Ill Patients: A Randomized Clinical Trial. JAMA. 2016;315:1480-90.
Moss M, Huang DT, Brower RG, Ferguson ND, Ginde AA, Gong MN, et al. Early Neuromuscular Blockade in the Acute Respiratory Distress Syndrome. The New England Journal of Medicine. 2019;380:1997-2008.
Papazian L, Forel J-M, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, et al. Neuromuscular Blockers in Early Acute Respiratory Distress Syndrome. New England Journal of Medicine. 2010;363:1107-16.
Yoshida T, Kavanagh BP, Brochard L. Early Neuromuscular Blockade in the Acute Respiratory Distress Syndrome. The New England Journal of Medicine. 2019;381:786-7.
Olsen HT, Nedergaard HK, Strøm T, Oxlund J, Wian K-A, Ytrebø LM, et al. Nonsedation or Light Sedation in Critically Ill, Mechanically Ventilated Patients. The New England Journal of Medicine. 2020;382:1103-11.
Ioannidis JPA. Why most discovered true associations are inflated. Epidemiology (Cambridge, Mass.). 2008;19:640-8.
Nedergaard HK, Korkmaz S, Olsen HT, Jensen HI, Strøm T, Toft P. Failure of non-sedation strategy in critically ill, mechanically ventilated patients - a retrospective, post-hoc analysis of the NONSEDA trial. Journal of Critical Care. 2022;68:66-71.
Sinclair MD. A review of the physiological effects of alpha2-agonists related to the clinical use of medetomidine in small animal practice. The Canadian Veterinary Journal = La Revue Veterinaire Canadienne. 2003;44:885-97.
Paris A, Tonner PH. Dexmedetomidine in anaesthesia. Current Opinion in Anaesthesiology. 2005;18:412-8.
Nelson LE, Lu J, Guo T, Saper CB, Franks NP, Maze M. The alpha2-adrenoceptor agonist dexmedetomidine converges on an endogenous sleep-promoting pathway to exert its sedative effects. Anesthesiology. 2003;98:428-36.
Aantaa R, Marjamäki A, Scheinin M. Molecular Pharmacology of α 2 -adrenoceptor Subtypes. Annals of Medicine. 1995;27:439-49.
Fairbanks CA, Stone LS, Wilcox GL. Pharmacological profiles of alpha 2 adrenergic receptor agonists identified using genetically altered mice and isobolographic analysis. Pharmacology & Therapeutics. 2009;123:224-38.
Reade MC, Eastwood GM, Bellomo R, Bailey M, Bersten A, Cheung B, et al. Effect of Dexmedetomidine Added to Standard Care on Ventilator-Free Time in Patients With Agitated Delirium: A Randomized Clinical Trial. JAMA. 2016;315:1460-8.
Skrobik Y, Duprey MS, Hill NS, Devlin JW. Low-Dose Nocturnal Dexmedetomidine Prevents ICU Delirium. A Randomized, Placebo-controlled Trial. American Journal of Respiratory and Critical Care Medicine. 2018;197:1147-56.
Jakob SM, Ruokonen E, Grounds RM, Sarapohja T, Garratt C, Pocock SJ, et al. Dexmedetomidine vs midazolam or propofol for sedation during prolonged mechanical ventilation: two randomized controlled trials. JAMA. 2012;307:1151-60.
Lankadeva YR, Shehabi Y, Deane AM, Plummer MP, Bellomo R, May CN. Emerging benefits and drawbacks of α 2 ‐adrenoceptor agonists in the management of sepsis and critical illness. British Journal of Pharmacology. 2021;178:1407-25.
Tracey KJ. Physiology and immunology of the cholinergic antiinflammatory pathway. The Journal of Clinical Investigation. 2007;117:289-96.
Hofer S, Steppan J, Wagner T, Funke B, Lichtenstern C, Martin E, et al. Central sympatholytics prolong survival in experimental sepsis. Critical Care (London, England). 2009;13:R11.
Calzavacca P, Booth LC, Lankadeva YR, Bailey SR, Burrell LM, Bailey M, et al. Effects of Clonidine on the Cardiovascular, Renal, and Inflammatory Responses to Experimental Bacteremia. Shock (Augusta, Ga.). 2019;51:348-55.
Kawazoe Y, Miyamoto K, Morimoto T, Yamamoto T, Fuke A, Hashimoto A, et al. Effect of Dexmedetomidine on Mortality and Ventilator-Free Days in Patients Requiring Mechanical Ventilation With Sepsis: A Randomized Clinical Trial. JAMA. 2017;317:1321-8.
Ohta Y, Miyamoto K, Kawazoe Y, Yamamura H, Morimoto T. Effect of dexmedetomidine on inflammation in patients with sepsis requiring mechanical ventilation: a sub-analysis of a multicenter randomized clinical trial. Critical Care (London, England). 2020;24:493.
Hong M, Milne B, Loomis C, Jhamandas K. Stereoselective effects of central alpha 2-adrenergic agonist medetomidine on in vivo catechol activity in the rat rostral ventrolateral medulla (RVLM). Brain Research. 1992;592:163-9.
Allen AM, Guyenet PG. Alpha 2-adrenoceptor-mediated inhibition of bulbospinal barosensitive cells of rat rostral medulla. The American Journal of Physiology. 1993;265:R1065-75.
Shirasaka T, Qiu D-L, Kannan H, Takasaki M. The effects of centrally administered dexmedetomidine on cardiovascular and sympathetic function in conscious rats. Anesthesia and Analgesia. 2007;105:1722-8, table of contents.
Kumar A, Haery C, Parrillo JE. Myocardial dysfunction in septic shock: Part I. Clinical manifestation of cardiovascular dysfunction. Journal of Cardiothoracic and Vascular Anesthesia. 2001;15:364-76.
Aninat C, Seguin P, Descheemaeker P-N, Morel F, Malledant Y, Guillouzo A. Catecholamines induce an inflammatory response in human hepatocytes. Critical Care Medicine. 2008;36:848-54.
De Backer D, Donadello K, Sakr Y, Ospina-Tascon G, Salgado D, Scolletta S, et al. Microcirculatory alterations in patients with severe sepsis: impact of time of assessment and relationship with outcome. Critical Care Medicine. 2013;41:791-9.
Martelli D, Yao ST, McKinley MJ, McAllen RM. Reflex control of inflammation by sympathetic nerves, not the vagus. The Journal of Physiology. 2014;592:1677-86.
Lankadeva YR, May CN, McKinley MJ, Neeland MR, Ma S, Hocking DM, et al. Sympathetic nerves control bacterial clearance. Scientific Reports. 2020;10:15009.
Andreis DT, Singer M. Catecholamines for inflammatory shock: a Jekyll-and-Hyde conundrum. Intensive Care Medicine. 2016;42:1387-97.
Weerink MAS, Struys MMRF, Hannivoort LN, Barends CRM, Absalom AR, Colin P. Clinical Pharmacokinetics and Pharmacodynamics of Dexmedetomidine. Clinical Pharmacokinetics. 2017;56:893-913.
Sharp DB, Wang X, Mendelowitz D. Dexmedetomidine decreases inhibitory but not excitatory neurotransmission to cardiac vagal neurons in the nucleus ambiguus. Brain Research. 2014;1574:1-5.
Ramchandra R, Wan L, Hood SG, Frithiof R, Bellomo R, May CN. Septic shock induces distinct changes in sympathetic nerve activity to the heart and kidney in conscious sheep. American Journal of Physiology. Regulatory, Integrative and Comparative Physiology. 2009;297:R1247-53.
Lewis K, Alshamsi F, Carayannopoulos KL, Granholm A, Piticaru J, Al Duhailib Z, et al. Dexmedetomidine vs other sedatives in critically ill mechanically ventilated adults: a systematic review and meta-analysis of randomized trials. Intensive Care Medicine. 2022;48:811-40.
Shehabi Y, Botha JA, Boyle MS, Ernest D, Freebairn RC, Jenkins IR, et al. Sedation and Delirium in the Intensive Care Unit: An Australian and New Zealand Perspective. Anaesthesia and Intensive Care. 2008;36:570-8.
Shehabi Y. Goals of goal-directed sedation. Revista Brasileira de Terapia Intensiva. 2015;27.
Shehabi Y, Howe BD, Bellomo R, Arabi YM, Bailey M, Bass FE, et al. Early Sedation with Dexmedetomidine in Critically Ill Patients. New England Journal of Medicine. 2019;380:2506-17.
Angus DC, Chang C-CH. Heterogeneity of Treatment Effect: Estimating How the Effects of Interventions Vary Across Individuals. JAMA. 2021;326:2312.
Shehabi Y, Serpa Neto A, Howe BD, Bellomo R, Arabi YM, Bailey M, et al. Early sedation with dexmedetomidine in ventilated critically ill patients and heterogeneity of treatment effect in the SPICE III randomised controlled trial. Intensive Care Medicine. 2021;47:455-66.
Shehabi Y, Serpa Neto A, Bellomo R, Howe BD, Arabi YM, Bailey M, et al. Dexmedetomidine and Propofol Sedation in Critically Ill Patients and Dose-associated 90-Day Mortality: A Secondary Cohort Analysis of a Randomized Controlled Trial (SPICE III). American Journal of Respiratory and Critical Care Medicine. 2023;207:876-86.
Kalil AC, Sun J. Why Are Clinicians Not Embracing the Results from Pivotal Clinical Trials in Severe Sepsis? A Bayesian Analysis. PLoS ONE. 2008;3:e2291.
Bray R, Hartley A, Wenkert D, Muehlemann N, Natanegara F, Harrell FE, et al. Why are There not More Bayesian Clinical Trials? Ability to Interpret Bayesian and Conventional Statistics Among Medical Researchers. Therapeutic Innovation & Regulatory Science. 2023;57:426-35.
Clark J, Muhlemann N, Natanegara F, Hartley A, Wenkert D, Wang F, et al. Why are not There More Bayesian Clinical Trials? Perceived Barriers and Educational Preferences Among Medical Researchers Involved in Drug Development. Therapeutic Innovation & Regulatory Science. 2023;57:417-25.
Zampieri FG, Damiani LP, Bakker J, Ospina-Tascón GA, Castro R, Cavalcanti AB, et al. Effects of a Resuscitation Strategy Targeting Peripheral Perfusion Status versus Serum Lactate Levels among Patients with Septic Shock. A Bayesian Reanalysis of the ANDROMEDA-SHOCK Trial. American Journal of Respiratory and Critical Care Medicine. 2020;201:423-9.
Goligher EC, Tomlinson G, Hajage D, Wijeysundera DN, Fan E, Jüni P, et al. Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome and Posterior Probability of Mortality Benefit in a Post Hoc Bayesian Analysis of a Randomized Clinical Trial. JAMA. 2018;320:2251-9.
Cioccari L, Luethi N, Bailey M, Shehabi Y, Howe B, Messmer AS, et al. The effect of dexmedetomidine on vasopressor requirements in patients with septic shock: a subgroup analysis of the Sedation Practice in Intensive Care Evaluation [SPICE III] Trial. Critical Care. 2020;24:441.
Amato MBP, Meade MO, Slutsky AS, Brochard L, Costa ELV, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. The New England Journal of Medicine. 2015;372:747-55.
VanderWeele TJ, Ding P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Annals of Internal Medicine. 2017;167:268.
Haneuse S, VanderWeele TJ, Arterburn D. Using the E-Value to Assess the Potential Effect of Unmeasured Confounding in Observational Studies. JAMA. 2019;321:602-3.
Shehabi Y, Thomson Z, Peppin C. SPICE IV Study: Early Sedation with Dexmedetomidine vs. Placebo in Older Ventilated Critically Ill Patients. School of Clinical Sciences at Monash Health Faculty of Medicine, Nursing & Health Sciences, Monash University. 2022.
Lee SJ, Lindquist K, Segal MR, Covinsky KE. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295:801-8.
Ouimet S, Kavanagh BP, Gottfried SB, Skrobik Y. Incidence, risk factors and consequences of ICU delirium. Intensive Care Medicine. 2007;33:66-73.
Liu H, Ji F, Peng K, Applegate RL, Fleming N. Sedation After Cardiac Surgery: Is One Drug Better Than Another? Anesthesia and Analgesia. 2017;124:1061-70.
Vissers KCP, Besse K, Hans G, Devulder J, Morlion B. Opioid rotation in the management of chronic pain: where is the evidence? Pain Practice: The Official Journal of World Institute of Pain. 2010;10:85-93.
Kirwan CJ, MacPhee IaM, Lee T, Holt DW, Philips BJ. Acute kidney injury reduces the hepatic metabolism of midazolam in critically ill patients. Intensive Care Medicine. 2012;38:76-84.
Philips BJ, Lane K, Dixon J, Macphee I. The effects of acute renal failure on drug metabolism. Expert Opinion on Drug Metabolism & Toxicology. 2014;10:11-23.
Conti G, Ranieri VM, Costa R, Garratt C, Wighton A, Spinazzola G, et al. Effects of dexmedetomidine and propofol on patient-ventilator interaction in difficult-to-wean, mechanically ventilated patients: a prospective, open-label, randomised, multicentre study. Critical Care (London, England). 2016;20:206.
Assadoon MS, Kovacevic MP, Dube KM, Szumita PM, Lupi KE, DeGrado JR. Evaluation of Atypical Antipsychotics for the Facilitation of Weaning Sedation in Mechanically Ventilated Critically Ill Patients. Journal of Intensive Care Medicine 2023. http://dx.doi.org/10.1177/08850666231188029.8850666231188029.
Stollings JL, Devlin JW, Lin JC, Pun BT, Byrum D, Barr J. Best Practices for Conducting Interprofessional Team Rounds to Facilitate Performance of the ICU Liberation (ABCDEF) Bundle. Critical Care Medicine. 2020;48:562-70.
Ten Hoorn S, Elbers PW, Girbes AR, Tuinman PR. Communicating with conscious and mechanically ventilated critically ill patients: a systematic review. Critical Care (London, England). 2016;20:333.
McRae J, Smith C, Emmanuel A, Beeke S. The experiences of individuals with cervical spinal cord injury and their family during post-injury care in non-specialised and specialised units in UK. BMC health services research. 2020;20:783.
Investigators TS, the ACTG, Hodgson CL, Bailey M, Bellomo R, Brickell K, et al. Early Active Mobilization during Mechanical Ventilation in the ICU. The New England Journal of Medicine. 2022;387:1747-58.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




