Neuromonitoring in neurocritical care for traumatic brain injury in the Thai context
Neuromonitoring for traumatic brain injury in Thailand
DOI:
https://doi.org/10.54205/ccc.v32.267083Keywords:
Traumatic brain injury, Neuro-monitoring, Cerebral Autoregulation, Cerebral homeostasis, Secondary brain injuryAbstract
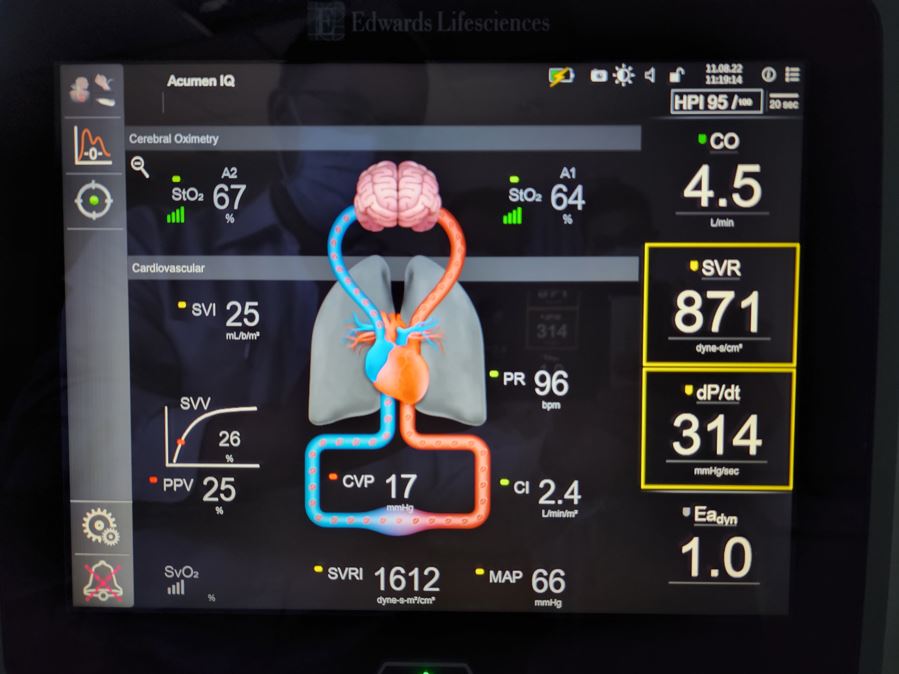
The purposes of this review were to identify the incidence and types of traumatic brain injury (TBI) in Thailand, and recommend neuro-monitoring for limited resources in Thai patients. The monitoring methods focus on the targeted and personalized management in severe TBI such as intracranial pressure (ICP), pressure reactivity index (PRx), regional cerebral saturation (rSO2), cerebral autoregulation (CA), as well as noninvasive methods for example near-infrared spectroscopy (NIRS) and optic nerve sheath diameter (ONSD). These monitors are aimed to optimize brain oxygen delivery and prevent further neurologic deterioration in terms of increased ICP and decreased cerebral perfusion pressure (CPP). Some of these were implemented in neurological monitoring protocol and clinical practice guidelines for severe TBI. However, cost - effectiveness is concerned. Even though considering CA and the advance monitoring methods in continuous assessment are widely used, current therapeutic interventions which appear entirely to bedside approach for correct dysregulated CA are limited. In addition, understanding of basic molecular and cellular pathways involved in cerebral homeostasis ( brain oxygen delivery, cerebral blood flow, CA and cerebral vascular reactivity to oxygen and carbon dioxide) as well as secondary brain injury prevention are still necessary for improving TBI outcomes. In summary, further study in Thailand is required to determine optimal cerebral physiologic-based technology, monitoring parameters, and individualized thresholds to optimize CA and potentially improve neurologic outcomes across a spectrum of TBI patients, which focus in Thai rural areas where invasive monitoring is not routinely performed due to resources limitation. Encourage and training of non invasive methods might solve these issues.
Downloads
References
Svedung Wettervik TM, Lewen A, Enblad P. Fine tuning of traumatic brain injury management in neurointensive care-indicative observations and future perspectives. Front Neurol. 2021;12:638132.
Somprasong T, et al. Thailand trauma statistics (In-hospital database) in 12 Health Regions of Ministry of Public Health: Ministry of Public Health report Nov. 2023;11-13.
Siripituphum D, Songwathana P, Khupantavee N, Williams I. Caring for Thai traumatic brain injury survivors in a transitional period: What are the barriers? Journal of Health Science and Medical Research. 2020;38(1), 43-52.
Sobut P. Factors predicting mortality in the patients with moderate to severe traumatic brain injury. NJPH. 2023;33(2):55-70.
Suvitsakulwong N, Phuangphung P. The study of the characters of traumatic brain injuries (TBI) in blunt head trauma caused by velocity-related injuries. Vajira Med J [Internet]. 2022;66(3):199-210.
Rubiano AM, Griswold DP, Jibaja M, Rabinstein AA, Godoy DA. Management of severe traumatic brain injury in regions with limited resources. Brain Inj. 2021;35:1317-25.
Gomez A, Sekhon M, Griesdale D, Froese L, Yang E, Thelin EP, et al. Cerebrovascular pressure reactivity and brain tissue oxygen monitoring provide complementary information regarding the lower and upper limits of cerebral blood flow control in traumatic brain injury: a CAnadian High Resolution-TBI (CAHR-TBI) cohort study. Intensive Care Med Exp. 2022;10:54.
Svedung Wettervik T, Howells T, Hillered L, Rostami E, Lewen A, Enblad P. Autoregulatory or fixed cerebral perfusion pressure targets in traumatic brain injury: Determining which is better in an energy metabolic perspective. J Neurotrauma. 2021;38:1969-78.
Tas J, Beqiri E, van Kaam RC, Czosnyka M, Donnelly J, Haeren RH, et al. Targeting autoregulation-guided cerebral perfusion pressure after traumatic brain injury (COGiTATE): A feasibility randomized controlled clinical trial. J Neurotrauma. 2021;38:2790-800.
Svedung Wettervik T, Hanell A, Howells T, Ronne Engstrom E, Lewen A, Enblad P. ICP, CPP, and PRx in traumatic brain injury and aneurysmal subarachnoid hemorrhage: association of insult intensity and duration with clinical outcome. J Neurosurg. 2023;138:446-53.
Zeiler FA, Donnelly J, Smielewski P, Menon DK, Hutchinson PJ, Czosnyka M. Critical Thresholds of intracranial pressure-derived continuous cerebrovascular reactivity indices for outcome prediction in noncraniectomized patients with traumatic brain injury. J Neurotrauma. 2018;35:1107-15.
Godoy DA, Rabinstein AA. How to manage traumatic brain injury without invasive monitoring? Curr Opin Crit Care. 2022;28:111-22.
Hawryluk GWJ, Citerio G, Hutchinson P, Kolias A, Meyfroidt G, Robba C, et al. Intracranial pressure: current perspectives on physiology and monitoring. Intensive Care Med. 2022;48:1471-81.
Brasil S, Godoy DA, Hawryluk GWJ. A Point-of-care noninvasive technique for surrogate ICP waveforms application in neurocritical care. Neurocrit Care. 2024;40:170-6.
Vitt JR, Loper NE, Mainali S. Multimodal and autoregulation monitoring in the neurointensive care unit. Front Neurol. 2023;14:1155986.
Muller SJ, Henkes E, Gounis MJ, Felber S, Ganslandt O, Henkes H. Non-invasive intracranial pressure monitoring. J Clin Med. 2023;12.
Robba C, Santori G, Czosnyka M, Corradi F, Bragazzi N, Padayachy L, et al. Optic nerve sheath diameter measured sonographically as non-invasive estimator of intracranial pressure: a systematic review and meta-analysis. Intensive Care Med. 2018;44:1284-94.
Girisgin AS, Kalkan E, Kocak S, Cander B, Gul M, Semiz M. The role of optic nerve ultrasonography in the diagnosis of elevated intracranial pressure. Emerg Med J. 2007;24:251-4.
Lee SH, Kim HS, Yun SJ. Optic nerve sheath diameter measurement for predicting raised intracranial pressure in adult patients with severe traumatic brain injury: A meta-analysis. J Crit Care. 2020;56:182-7.
Kim DY, Kim SY, Hong DY, Sung BY, Lee S, Paik JH, et al. Comparison of ultrasonography and computed tomography for measuring optic nerve sheath diameter for the detection of elevated intracranial pressure. Clin Neurol Neurosurg. 2021;204:106609.
Stevens RRF, Gommer ED, Aries MJH, Ertl M, Mess WH, Huberts W, et al. Optic nerve sheath diameter assessment by neurosonology: A review of methodologic discrepancies. J Neuroimaging. 2021;31:814-25.
Rajajee V, Vanaman M, Fletcher JJ, Jacobs TL. Optic nerve ultrasound for the detection of raised intracranial pressure. Neurocrit Care. 2011;15:506-15.
Aletreby W, Alharthy A, Brindley PG, Kutsogiannis DJ, Faqihi F, Alzayer W, et al. Optic Nerve Sheath Diameter Ultrasound for Raised Intracranial Pressure: A Literature Review and Meta-analysis of its Diagnostic Accuracy. J Ultrasound Med. 2022;41:585-95.
De Bernardo M, Rosa N. Comment on 'Invasive and noninvasive means of measuring intracranial pressure: a review'. Physiol Meas. 2018;39:058001.
Iaconetta G, De Bernardo M, Rosa N. Coronal axis measurement of the optic nerve sheath diameter. J Ultrasound Med. 2017;36:1073.
de Courson H, Proust-Lima C, Tuaz E, Georges D, Verchere E, Biais M. Relationship between brain tissue oxygen and near-infrared spectroscopy in patients with nontraumatic subarachnoid hemorrhage. Neurocrit Care. 2022;37:620-8.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




