The efficacy of P0.1-guided sedation protocol in critically ill patients receiving invasive mechanical ventilation: A randomized controlled trial
The efficacy of P0.1-guided sedation in mechanically ventilated patients
DOI:
https://doi.org/10.54205/ccc.v32.268622Keywords:
Acute respiratory failure, Mechanical ventilation, P0.1, Respiratory drive, SedationAbstract
Background: Mechanical ventilation is a lifesaving treatment in patients with acute respiratory failure. Despite optimal support, some patients still exhibit excessive respiratory drive, leading to patient self-inflicted lung injury (P-SILI) and diaphragmatic dysfunction. Sedation and muscle relaxants are commonly used to reduce respiratory efforts and manage patient-ventilator asynchrony (PVA). Conventionally, sedative drugs are adjusted based on the sedation level assessed by the Richmond Agitation-Sedation Scale (RASS), which may not correlate with the patient’s respiratory drive. Drop in airway pressure at the first 100 milliseconds of the beginning of the inspiration after the end-expiratory occlusion (P0.1) is a simple and reliable method of respiratory drive monitoring by mechanical ventilation at the bedside and may be the more suitable sedation target.
Objectives: To assess the efficacy of a sedation protocol targeting optimal P0.1 and RASS score compared to conventional sedation strategy in patients requiring invasive mechanical ventilation in the medical intensive care units in terms of successful extubation.
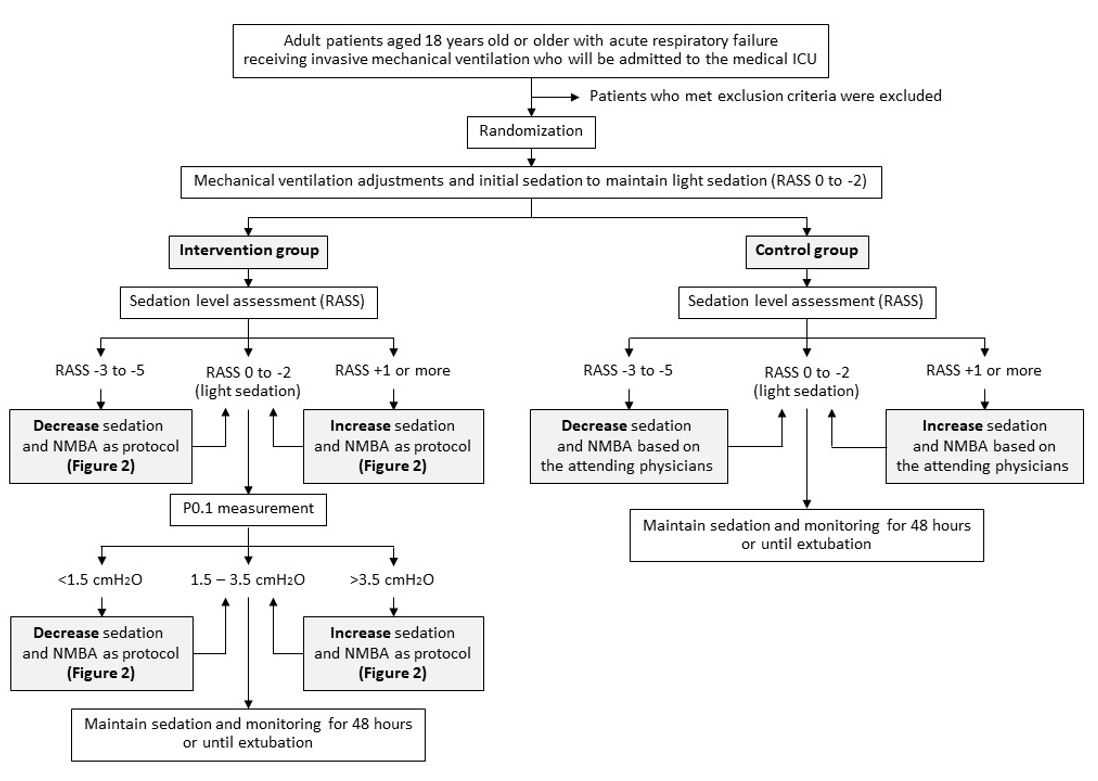
Methods: This is an open-labeled, single-center, randomized controlled trial conducted in medical intensive care units at a tertiary care hospital in Bangkok, Thailand. We randomly allocated mechanically ventilated patients in a 1:1 ratio to receive a sedation protocol targeting both optimal respiratory drive measured by P0.1 (intervention group) and light sedation (RASS 0 to -2) or standard of care (control group targeting RASS alone). The primary outcome is the rate of successful extubation within 14 days after randomization.
Hypothesis: We hypothesize that sedation protocol targeting optimal P0.1 and light sedation will increase the rate of successful extubation at 14 days in mechanically ventilated patients compared to conventional sedation strategy.
Conclusions: This study aims to evaluate the efficacy of a sedation protocol using P0.1 measurement to monitor and target optimal respiratory drive, in conjunction with sedation scores, in critically ill patients receiving invasive mechanical ventilation.
Ethics and dissemination: This study protocol was approved by the Human Research Protection Unit of the Faculty of Medicine, Siriraj Hospital, Mahidol University (Certificate of Approval no. Si 915/2023).
Trial registration: NCT06203405
Downloads
References
Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017;195:438-42.
Sklienka P, Frelich M, Burša F. Patient self-inflicted lung injury-A narrative review of pathophysiology, early recognition, and management options. J Pers Med. 2023;13.
Carteaux G, Parfait M, Combet M, Haudebourg AF, Tuffet S, Mekontso Dessap A. Patient-self inflicted lung injury: A practical review. J Clin Med. 2021;10.
Spinelli E, Mauri T, Beitler JR, Pesenti A, Brodie D. Respiratory drive in the acute respiratory distress syndrome: pathophysiology, monitoring, and therapeutic interventions. Intensive Care Med. 2020;46:606-18.
Spinelli E, Pesenti A, Slobod D, Fornari C, Fumagalli R, Grasselli G, et al. Clinical risk factors for increased respiratory drive in intubated hypoxemic patients. Crit Care. 2023;27:138.
Chanques G, Constantin JM, Devlin JW, Ely EW, Fraser GL, Gélinas C, et al. Analgesia and sedation in patients with ARDS. Intensive Care Med. 2020;46:2342-56.
Goligher EC, Jonkman AH, Dianti J, Vaporidi K, Beitler JR, Patel BK, et al. Clinical strategies for implementing lung and diaphragm-protective ventilation: avoiding insufficient and excessive effort. Intensive Care Med. 2020;46:2314-26.
Dzierba AL, Khalil AM, Derry KL, Madahar P, Beitler JR. Discordance between respiratory drive and sedation depth in critically ill patients receiving mechanical ventilation. Crit Care Med. 2021;49:2090-101.
Wongtangman K, Grabitz SD, Hammer M, Wachtendorf LJ, Xu X, Schaefer MS, et al. Optimal sedation in patients who receive neuromuscular blocking agent infusions for treatment of acute respiratory distress syndrome-A retrospective cohort study from A New England Health Care Network. Crit Care Med. 2021;49:1137-48.
Jackson DL, Proudfoot CW, Cann KF, Walsh TS. The incidence of sub-optimal sedation in the ICU: a systematic review. Crit Care. 2009;13:R204.
Kassis EB, Beitler JR, Talmor D. Lung-protective sedation: moving toward a new paradigm of precision sedation. Intensive Care Med. 2023;49:91-4.
Bertoni M, Spadaro S, Goligher EC. Monitoring patient respiratory effort during mechanical ventilation: Lung and diaphragm-protective ventilation. Crit Care. 2020;24:106.
Rittayamai N, Beloncle F, Goligher EC, Chen L, Mancebo J, Richard JM, et al. Effect of inspiratory synchronization during pressure-controlled ventilation on lung distension and inspiratory effort. Ann Intensive Care. 2017;7:100.
Telias I, Junhasavasdikul D, Rittayamai N, Piquilloud L, Chen L, Ferguson ND, et al. Airway occlusion pressure as an estimate of respiratory drive and inspiratory effort during assisted ventilation. Am J Respir Crit Care Med. 2020;201:1086-98.
Beloncle F, Piquilloud L, Olivier PY, Vuillermoz A, Yvin E, Mercat A, et al. Accuracy of P0.1 measurements performed by ICU ventilators: A bench study. Ann Intensive Care. 2019;9:104.
Theerawit P, Soipetkasem P. An importance of respiratory drive and effort during mechanical ventilation: Respiratory drive and effort in respiratory failure. Clinical Critical Care. 2023;31:2023:e0001.
de Vries HJ, Tuinman PR, Jonkman AH, Liu L, Qiu H, Girbes ARJ, et al. Performance of noninvasive airway occlusion maneuvers to assess lung stress and diaphragm effort in mechanically ventilated critically ill patients. Anesthesiology. 2023;138:274-88.
Grasselli G, Calfee CS, Camporota L, Poole D, Amato MBP, Antonelli M, et al. ESICM guidelines on acute respiratory distress syndrome: definition, phenotyping and respiratory support strategies. Intensive Care Med. 2023;49:727-59.
Brenner M, Mukai DS, Russell JE, Spiritus EM, Wilson AF. A new method for measurement of airway occlusion pressure. Chest. 1990;98:421-7.
Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJC, Pandharipande PP, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46:e825-e73.
Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41:263-306.
Seo Y, Lee HJ, Ha EJ, Ha TS. 2021 KSCCM clinical practice guidelines for pain, agitation, delirium, immobility, and sleep disturbance in the intensive care unit. Acute Crit Care. 2022;37:1-25.
Marra A, Ely EW, Pandharipande PP, Patel MB. The ABCDEF bundle in critical care. Crit Care Clin. 2017;33:225-43.
Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, et al. Weaning from mechanical ventilation. Eur Respir J. 2007;29:1033-56.
Tongyoo S, Tantibundit P, Daorattanachai K, Viarasilpa T, Permpikul C, Udompanturak S. High-flow nasal oxygen cannula vs. noninvasive mechanical ventilation to prevent reintubation in sepsis: A randomized controlled trial. Ann Intensive Care. 2021;11:135.
Sandhu RS, Pasquale MD, Miller K, Wasser TE. Measurement of endotracheal tube cuff leak to predict postextubation stridor and need for reintubation. J Am Coll Surg. 2000;190:682-7.
Pluijms WA, van Mook WN, Wittekamp BH, Bergmans DC. Postextubation laryngeal edema and stridor resulting in respiratory failure in critically ill adult patients: Updated review. Crit Care. 2015;19:295.
Hernández G, Vaquero C, Colinas L, Cuena R, González P, Canabal A, et al. Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients: A randomized clinical trial. Jama. 2016;316:1565-74.
Yehya N, Harhay MO, Curley MAQ, Schoenfeld DA, Reeder RW. Reappraisal of ventilator-free days in critical care research. Am J Respir Crit Care Med. 2019;200:828-36.
Tongyoo S, Viarasilpa T, Deawtrakulchai P, Subpinyo S, Suppasilp C, Permpikul C. Comparison of limited driving pressure ventilation and low tidal volume strategies in adults with acute respiratory failure on mechanical ventilation: A randomized controlled trial. Ther Adv Respir Dis. 2024;18:17534666241249152.
Cheng KC, Hou CC, Huang HC, Lin SC, Zhang H. Intravenous injection of methylprednisolone reduces the incidence of postextubation stridor in intensive care unit patients. Crit Care Med. 2006;34:1345-50.
Fan T, Wang G, Mao B, Xiong Z, Zhang Y, Liu X, et al. Prophylactic administration of parenteral steroids for preventing airway complications after extubation in adults: Meta-analysis of randomised placebo controlled trials. Bmj. 2008;337:a1841.
Lee CH, Peng MJ, Wu CL. Dexamethasone to prevent postextubation airway obstruction in adults: A prospective, randomized, double-blind, placebo-controlled study. Crit Care. 2007;11:R72.
Papazian L, Klompas M, Luyt CE. Ventilator-associated pneumonia in adults: A narrative review. Intensive Care Med. 2020;46:888-906.
Klompas M, Branson R, Cawcutt K, Crist M, Eichenwald EC, Greene LR, et al. Strategies to prevent ventilator-associated pneumonia, ventilator-associated events, and nonventilator hospital-acquired pneumonia in acute-care hospitals: 2022 Update. Infect Control Hosp Epidemiol. 2022;43:687-713.
Singh A, Anjankar AP. Propofol-related infusion syndrome: A clinical review. Cureus. 2022;14:e30383.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




