Comparison of guiding sedation level by respiratory effort versus usual care in mechanically ventilated patients: A randomized controlled trial protocol
The effect of sedation protocol guided by respiratory effort
DOI:
https://doi.org/10.54205/ccc.v32.268690Keywords:
Respiratory effort, Acute respiratory distress syndrome, Dynamic transpulmonary driving pressure swing, Sedation protocolAbstract
Background: Critically ill patients relying on mechanical ventilation often require excessive sedation, aiming to address asynchrony and prevent ventilator-induced lung injury (VILI). Unintentionally, there may be more suppression of respiratory efforts. It is well-established that improper respiratory efforts during mechanical ventilation can cause unfavorable outcomes.
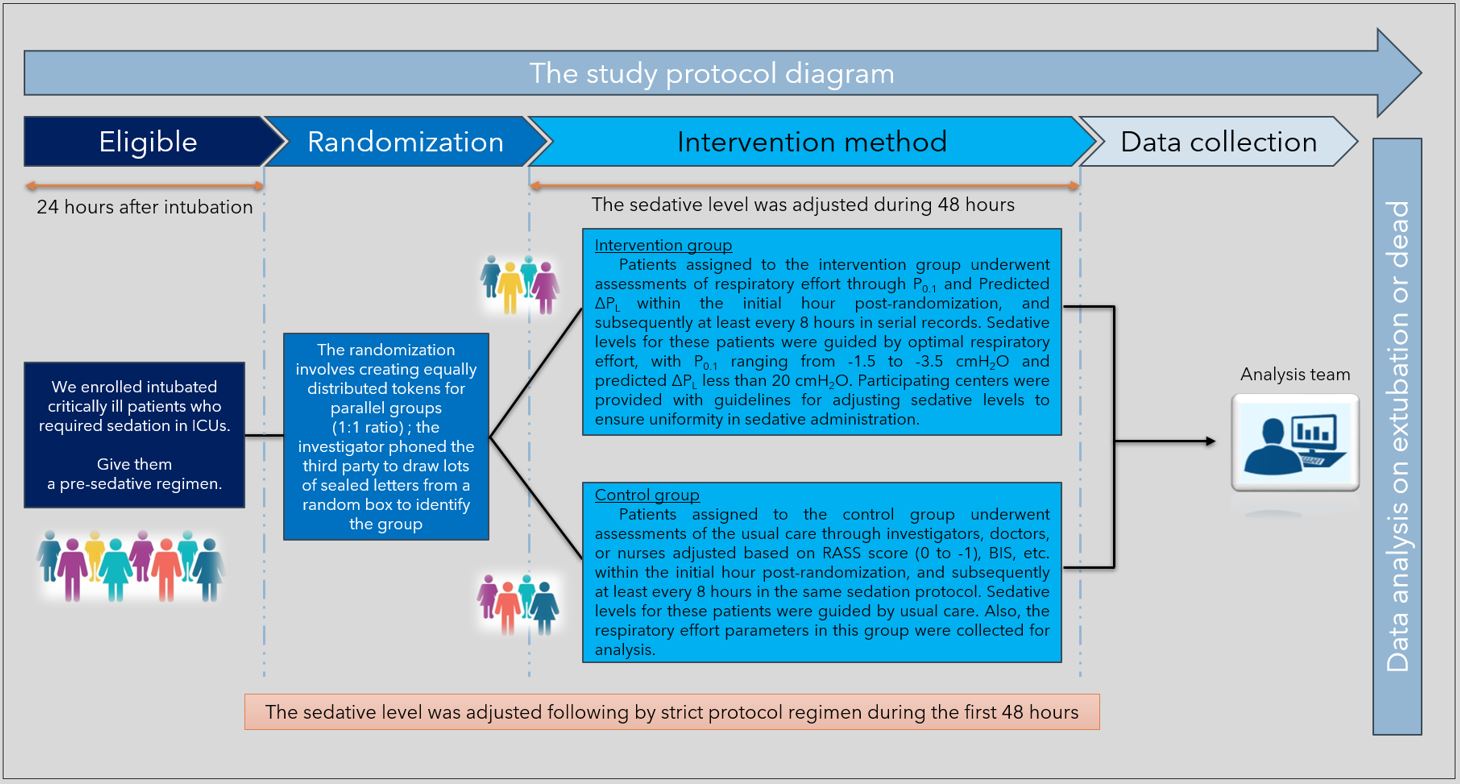
Methods: Researchers conducted a single-center randomized control trial, parallel 2 groups (1:1 ratio), with 164 participants. One intervention group employed the optimal respiratory effort (predicted ΔPL, P0.1), and the other control group, employed usual care to guide the adjustment of sedative levels.
Hypothesis: To compare 28-day ventilator-free day (VFD) and mortality between measuring respiratory effort as opposed to usual care and adjusting sedative level during mechanical ventilation.
Conclusions: This study will evaluate the disparity in 28-day VFD and mortality between sedative level guidance by respiratory effort and usual care.
Ethics and dissemination: The study protocol received approval from the Human Research Ethics Committee, Faculty of Medicine Ramathibodi Hospital, Mahidol University (COA No. MURA2023/642)
Trial registration: NCT06242236
Downloads
References
Orozco-Levi M, Lloreta J, Minguella J, Serrano S, Broquetas JM, Gea J. Injury of the human diaphragm associated with exertion and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;164:1734-9.
Scott A, Wang X, Road JD, Reid WD. Increased injury and intramuscular collagen of the diaphragm in COPD: autopsy observations. Eur Respir J. 2006;27:51-9.
Loeb L. The Mechanism in the development of pulmonary edema. Proceedings of the society for experimental biology and medicine. 1928;25:321-3.
Moore RL, Binger CA. The response to respiratory resistance : a comparison of the effects produced by partial obstruction in the inspiratory and expiratory phases of respiration. J Exp Med. 1927;45:1065-80.
Barach AL, Eckman M. The effects of inhalation of helium mixed with oxygen on the mechanics of respiration. J Clin Invest. 1936;15:47-61.
Dreyfuss D, Soler P, Basset G, Saumon G. High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis. 1988;137:1159-64.
Mascheroni D, Kolobow T, Fumagalli R, Moretti MP, Chen V, Buckhold D. Acute respiratory failure following pharmacologically induced hyperventilation: An experimental animal study. Intensive Care Med. 1988;15:8-14.
Yoshida T, Uchiyama A, Matsuura N, Mashimo T, Fujino Y. The comparison of spontaneous breathing and muscle paralysis in two different severities of experimental lung injury. Crit Care Med. 2013;41:536-45.
Yoshida T, Torsani V, Gomes S, De Santis RR, Beraldo MA, Costa EL, et al. Spontaneous effort causes occult pendelluft during mechanical ventilation. Am J Respir Crit Care Med. 2013;188:1420-7.
Goligher EC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, et al. Mechanical ventilation-induced diaphragm atrophy strongly impacts clinical outcomes. Am J Respir Crit Care Med. 2018;197:204-13.
Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, et al. The richmond agitation-sedation scale: Validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166:1338-44.
Taran Z, Namadian M, Faghihzadeh S, Naghibi T. The Effect of sedation protocol using Richmond Agitation-Sedation Scale (RASS) on some clinical outcomes of mechanically ventilated patients in intensive care units: A randomized clinical trial. J Caring Sci. 2019;8:199-206.
Dzierba AL, Khalil AM, Derry KL, Madahar P, Beitler JR. Discordance between respiratory drive and sedation depth in critically ill patients receiving mechanical ventilation. Crit Care Med. 2021;49:2090-101.
Bertoni M, Telias I, Urner M, Long M, Del Sorbo L, Fan E, et al. A novel non-invasive method to detect excessively high respiratory effort and dynamic transpulmonary driving pressure during mechanical ventilation. Crit Care. 2019;23:346.
Bertoni M, Spadaro S, Goligher EC. Monitoring patient respiratory effort during mechanical ventilation: Lung and diaphragm-protective ventilation. Crit Care. 2020;24:106.
Bellani G, Grasselli G, Teggia-Droghi M, Mauri T, Coppadoro A, Brochard L, et al. Do spontaneous and mechanical breathing have similar effects on average transpulmonary and alveolar pressure? A clinical crossover study. Crit Care. 2016;20:142.
Baedorf Kassis E, Loring SH, Talmor D. Mortality and pulmonary mechanics in relation to respiratory system and transpulmonary driving pressures in ARDS. Intensive Care Med. 2016;42:1206-13.
Spinelli E, Pesenti A, Slobod D, Fornari C, Fumagalli R, Grasselli G, et al. Clinical risk factors for increased respiratory drive in intubated hypoxemic patients. Crit Care. 2023;27:138.
Spinelli E, Mauri T, Beitler JR, Pesenti A, Brodie D. Respiratory drive in the acute respiratory distress syndrome: pathophysiology, monitoring, and therapeutic interventions. Intensive Care Med. 2020;46:606-18.
Ouellette DR, Patel S, Girard TD, Morris PE, Schmidt GA, Truwit JD, et al. Liberation from mechanical ventilation in critically ill adults: An official american college of chest physicians/american thoracic society clinical practice guideline: Inspiratory pressure augmentation during spontaneous breathing trials, protocols minimizing sedation, and noninvasive ventilation immediately after extubation. Chest. 2017;151(1):166-180.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




