Platypnea and orthodeoxia syndrome due to a right-to-left shunt via the foramen ovale in the absence of pulmonary hypertension after orthotopic liver transplantation: Sequelae leading to brain abscess: A case report
Reopening foramen ovale in the absence of pulmonary hypertension causes POS and brain abscess after orthotopic liver transplantation
DOI:
https://doi.org/10.54205/ccc.v33.273699Keywords:
Platypnea and orthodeoxia syndrome, Reopen PFO without pulmonary hypertension, Brain abscess, Liver transplantationAbstract
Introduction: Platypnea and orthodeoxia syndrome (POS) refers to the worsening of dyspnea and desaturation in the upright position. The most common cause of POS is a right-to-left intra-cardiac shunt. Patent foramen ovale (PFO) is a remnant of normal fetal anatomy that can continue into adulthood. Most are asymptomatic as the pressure in the left atrium is higher than in the right atrium, leading to the functional closure of the foramen ovale.
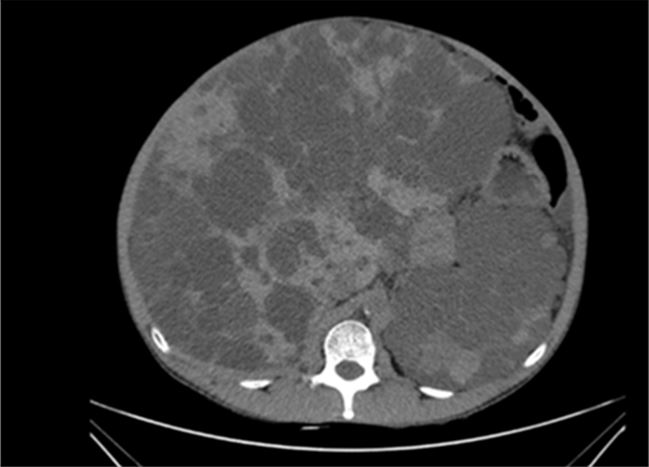
Case presentation: We report an autosomal dominant polycystic kidney and liver disease (ADPKD) patient with PFO Grade II–III, atrial septal aneurysm (ASA), and dilatation of the aortic root complicated with multiple dental caries and chronic gingivitis. He developed POS and brain abscess after liver and kidney transplantation. Right-to-left shunt was proved by the air contrast transesophageal echocardiography (TEE) review in the normal right atrium and pulmonary artery pressure. Concomitant cardiac pathology of ASA, dilatation of the aortic root, and elevation of the right hemidiaphragm after surgery might reposition the atrium septum and redirect inferior vena cava blood flow through PFO to the left atrium, causing reopening of PFO and right-to-left shunt. Multiple dental caries and chronic gingivitis might be the cause of brain abscess from paradoxical septic embolism. With the condition of complex and high-grade PFO and high Risk of Paradoxical Embolism (ROPE) score with POS, questions were raised concerning the closure of PFO either in the preoperative or especially postoperative period after POS was detected after liver transplantation to prevent paradoxical embolism. With the potential risk of complications with the closing of PFO, this issue should be addressed in a multidisciplinary approach, with the patient and family. However, aggressive treatment of intraoral infection is an important issue.
Conclusions: POS could happen in patient with underlying PFO associated with ASA undergoing orthotopic liver transplantation with elevation of right hemidiaphragm. Multidisplinary care team approach should be arranged for the decision of closure of this PFO to prevent intraoperative and serious postoperative complications.
Downloads
References
Salas-Pacheco JL. Mechanisms of platypnea-orthodeoxia syndrome. Arch Cardiol Mex. 2022;92:274-82.
Agrawal A, Palkar A, Talwar A. The multiple dimensions of Platypnea-Orthodeoxia syndrome: A review. Respir Med. 2017:129:31-8.
Abbas AE, Fortuin FD, Schiller NB, Appleton CP, Moreno CA, Lester SJ. A simple method for noninvasive estimation of pulmonary vascular resistance. J Am Coll Cardiol. 2003;41:1021-27.
Aragon Pinto C, Iyer VN, Albitar HAH, Anderson A, Cajigas H, Simonetto DA, et al. Outcomes of liver transplantation in patients with hepatopulmonary syndrome in the pre and post-MELD eras: A systematic review. Respir Med Res. 2021;80:100852.
Al-Saleh S, Mei-Zahav M, Faughnan ME, MacLusky IB, Carpenter S, Letarte M. Screening for pulmonary and cerebral arteriovenous malformations in children with hereditary haemorrhagic telangiectasia. Eur Respir J. 2009;34:875–81.
Zhang H, Bai C, Wang J, Han G, Guo X, Zhou X, et al. Significance of lung perfusion scanning with technetium labeled macroaggregated albumin and pulmonary function assay for diagnosis of early hepatopulmonary syndrome. Zhonghua Gan Zang Bing Za Zhi. 2001;9:331-3.
Teshome MK, Najib K, Nwagbara CC, Akinseye OA, Ibebuogu UN. Patent foramen ovale: a comprehensive review. Curr Probl Cardio. 2020;45:100392.
Bancal C, Arnoult F, Krapf L, Bonay M. Patent foramen ovale and hypoxaemia with or without elevated right heart pressures. Rev Mal Respir. 2011;28:967–77.
Eicher JC, Bonniaud P, Baudouin N, Petit A, Bertaux G, Donal E, et al. Hypoxaemia associated with an enlarged aortic root: a new syndrome? Heart 2005;91:1030-5.
Shakur R, Ryding A, Timperley J, Becher H, Leeson P. Late emergence of platypnea orthodeoxia: Chiari network and atrial septal hypertrophy demonstrated with transoesophageal echocardiography. Eur J Echocardiogr. 2008;9:694-6.
Sakagianni K, Evrenoglou D, Mytas D, Vavuranakis M, Platypnea-orthodeoxia syndrome related to right hemidiaphragmatic elevation and a 'stretched' patent foramen ovale. BMJ Case Rep. 2012;10:2012.
Soliman OII, Geleijnse ML, Meijboom FJ, Nemes A, Kamp O, Nihoyannopoulos P, et al. The use of contrast echocardiography for the detection of cardiac shunts. Eur J Echocardiogr. 2007;8:S2-12.
Horiuchi Y, Kato Y, Dembo T, Takeda H, Fukuoka T, Tanahashi N. Patent foramen ovale as a risk factor for cryptogenic brain abscess: case report and review of the literature. Intern Med. 2012;51:1111-4.
Shillcutt SK, Ringenberg KJ, Chacon MM, Brakke TR, Montzingo CR, Lyden ER, et al. Liver transplantation: intraoperative transesophageal echocardiography findings and relationship to major postoperative adverse cardiac events. J Cardiothorac Vasc Anesth. 2016;30:107-14.
Gertsvolf N, Andersen E, Othman T, Xu P, Phuong N, Butera B, et al. Patent foramen ovale and neurologic events in patients undergoing liver transplantation. Cardiovasc Revasc Med. 2018;19:53-5.
Lechat P, Mas JL, Lascault G, Loron P, Theard M, Klimczac M, et al. Prevalence of patent foramen ovale in patients with stroke. N Engl J Med. 1988;318:1148-52.
Jan F, Hafiz AM, Gupta S, Meidl J, Allaqaband S. Brain abscesses in a patient with a patent foramen ovale: a case report. J Med Case Rep. 2009;3:9299.
Akagi T. Transcatheter closure of patent foramen ovale: Current evidence and future perspectives. J Cardiol. 2021;77:3-9.
Messe SR, Gronseth GS, Kent DM, Kizer JR, Homma S, Rosterman L, et al. Practice advisory update summary: patent foramen ovale and secondary stroke prevention: report of the guideline subcommittee of the American Academy of Neurology. Neurology. 2020;94:876–85.
Kent DM, Thaler DE. The risk of paradoxical embolism (RoPE) study: developing risk models for application to ongoing randomized trials of percutaneous patent foramen ovale closure for cryptogenic stroke. Trials. 2011;12:185.
Kerut EK, Campbell WF, Hall ME, McMullan MR. Identification of candidates for PFO closure in the echocardiography laboratory. Echocardiography. 2018;35:1860-7.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




