Calcium channel blocker overdose in real world practice: A case report
Management for CCBs overdose
DOI:
https://doi.org/10.54205/ccc.v33.275336Keywords:
Calcium channel blockers toxicity, High-dose insulin euglycemia therapy, GI decontamination, Methylene blue, Intravenous lipid emulsion, Intensive care unitAbstract
Introduction: Calcium channel blocker (CCB) toxicity, particularly from dihydropyridine agents, like amlodipine, can cause life-threatening vasodilatory shock, bradycardia, and metabolic disturbances. In severe cases, standard resuscitative measures may be insufficient, necessitating advanced supportive and targeted therapies.
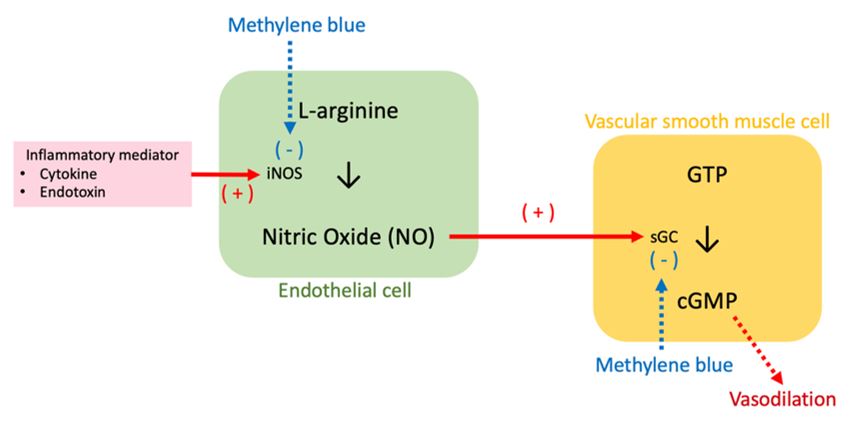
Case Presentation: A 72-year-old male presented 9 h after intentional ingestion of 200 tablets (1000 mg) of amlodipine with hypotension, metabolic acidosis, and acute kidney injury, but without hyperglycemia. Initial management included intravenous fluid resuscitation, calcium gluconate, and vasopressors. Despite this, he developed refractory shock, acute respiratory failure, and cardiac arrhythmia, requiring mechanical ventilation and intensive hemodynamic support. High-dose insulin euglycemia therapy (HIE) and methylene blue were administered. Renal function gradually improved, and vasopressors were weaned, and the patient was successfully extubated and discharged.
Conclusion: This case highlights the complexity of managing severe amlodipine overdose, emphasizing the role of early vasopressors, calcium salt administration, and adjunctive therapies such as HIE and methylene blue. Prompt recognition and a multimodal approach are critical for improving outcomes in patients with CCB toxicity.
Downloads
References
Chakraborty RK, Hamilton RJ. Calcium Channel Blocker Toxicity. StatPearls. Treasure Island (FL); 2025.
Goldfine CE, Troger A, Erickson TB, Chai PR. Beta-blocker and calcium-channel blocker toxicity: current evidence on evaluation and management. Eur Heart J Acute Cardiovasc Care. 2024;13:247-53.
Lheureux PE, Zahir S, Gris M, Derrey AS, Penaloza A. Bench-to-bedside review: hyperinsulinaemia/euglycaemia therapy in the management of overdose of calcium-channel blockers. Crit Care. 2006;10:212.
da Silva OA, de Melo RA, Jorge Filho JP. Verapamil acute self-poisoning. Clin Toxicol. 1979;14:361-7.
Pellegrini JR, Jr., Munshi R, Tiwana MS, Abraham T, Tahir H, Sayedy N, et al. "Feeling the Blues": A Case of Calcium Channel Blocker Overdose Managed With Methylene Blue. Cureus. 2021;13:e19114.
Levine M, Boyer EW, Pozner CN, Geib AJ, Thomsen T, Mick N, et al. Assessment of hyperglycemia after calcium channel blocker overdoses involving diltiazem or verapamil. Crit Care Med. 2007;35:2071-5.
Levine M, Curry SC, Padilla-Jones A, Ruha AM. Critical care management of verapamil and diltiazem overdose with a focus on vasopressors: a 25-year experience at a single center. Ann Emerg Med. 2013;62:252-8.
St-Onge M, Anseeuw K, Cantrell FL, Gilchrist IC, Hantson P, Bailey B, et al. Experts Consensus Recommendations for the Management of Calcium Channel Blocker Poisoning in Adults. Crit Care Med. 2017;45:e306-e15.
Fadhlillah F, Patil S. Pharmacological and mechanical management of calcium channel blocker toxicity. BMJ Case Rep. 2018;2018.
Alshaya OA, Alhamed A, Althewaibi S, Fetyani L, Alshehri S, Alnashmi F, et al. Calcium Channel Blocker Toxicity: A Practical Approach. J Multidiscip Healthc. 2022;15:1851-62.
Ramoska EA, Spiller HA, Winter M, Borys D. A one-year evaluation of calcium channel blocker overdoses: toxicity and treatment. Ann Emerg Med. 1993;22:196-200.
Rotella JA, Greene SL, Koutsogiannis Z, Graudins A, Hung Leang Y, Kuan K, et al. Treatment for beta-blocker poisoning: a systematic review. Clin Toxicol (Phila). 2020;58:943-83.
Lindeman E, Alebring J, Johansson A, Ahlner J, Kugelberg FC, Nordmark Grass J. The unknown known: non-cardiogenic pulmonary edema in amlodipine poisoning, a cohort study. Clin Toxicol (Phila). 2020;58:1042-9.
Izdes S, Altintas ND, Soykut C. Acute respiratory distress syndrome after verapamil intoxication: case report and literature review. Acta Clin Belg. 2014;69:116-9.
Barrow PM, Houston PL, Wong DT. Overdose of sustained-release verapamil. Br J Anaesth. 1994;72:361-5.
Lapatto-Reiniluoto O, Kivisto KT, Neuvonen PJ. Gastric decontamination performed 5 min after the ingestion of temazepam, verapamil and moclobemide: charcoal is superior to lavage. Br J Clin Pharmacol. 2000;49:274-8.
Benson BE, Hoppu K, Troutman WG, Bedry R, Erdman A, Hojer J, et al. Position paper update: gastric lavage for gastrointestinal decontamination. Clin Toxicol (Phila). 2013;51:140-6.
Kerns W, 2nd. Management of beta-adrenergic blocker and calcium channel antagonist toxicity. Emerg Med Clin North Am. 2007;25:309-31; abstract viii.
Engebretsen KM, Kaczmarek KM, Morgan J, Holger JS. High-dose insulin therapy in beta-blocker and calcium channel-blocker poisoning. Clin Toxicol (Phila). 2011;49:277-83.
Kline JA, Leonova E, Raymond RM. Beneficial myocardial metabolic effects of insulin during verapamil toxicity in the anesthetized canine. Crit Care Med. 1995;23:1251-63.
Kline JA, Raymond RM, Leonova ED, Williams TC, Watts JA. Insulin improves heart function and metabolism during non-ischemic cardiogenic shock in awake canines. Cardiovasc Res. 1997;34:289-98.
Page CB, Ryan NM, Isbister GK. The safety of high-dose insulin euglycaemia therapy in toxin-induced cardiac toxicity. Clin Toxicol (Phila). 2018;56:389-96.
Ahmed S, Barnes S. Hemodynamic improvement using methylene blue after calcium channel blocker overdose. World J Emerg Med. 2019;10:55-8.
Lenasi H, Kohlstedt K, Fichtlscherer B, Mulsch A, Busse R, Fleming I. Amlodipine activates the endothelial nitric oxide synthase by altering phosphorylation on Ser1177 and Thr495. Cardiovasc Res. 2003;59:844-53.
Pluta MP, Putowski Z, Czempik PF, Krzych LJ. Successful Use of Methylene Blue in Catecholamine-Resistant Septic Shock: A Case Report and Short Literature Review. Int J Mol Sci. 2023;24.
Saha BK, Bonnier A, Chong W. Rapid reversal of vasoplegia with methylene blue in calcium channel blocker poisoning. Afr J Emerg Med. 2020;10:284-7.
Rutledge C, Brown B, Benner K, Prabhakaran P, Hayes L. A Novel Use of Methylene Blue in the Pediatric ICU. Pediatrics. 2015;136:e1030-4.
Curry S. Methemoglobinemia. Ann Emerg Med. 1982;11:214-21.
Turner-Lawrence DE, Kerns Ii W. Intravenous fat emulsion: a potential novel antidote. J Med Toxicol. 2008;4:109-14.
Lekka ME, Liokatis S, Nathanail C, Galani V, Nakos G. The impact of intravenous fat emulsion administration in acute lung injury. Am J Respir Crit Care Med. 2004;169:638-44.
American College of Medical T. ACMT Position Statement: Guidance for the Use of Intravenous Lipid Emulsion. J Med Toxicol. 2017;13:124-5.
Fettiplace MR, Akpa BS, Rubinstein I, Weinberg G. Confusion About Infusion: Rational Volume Limits for Intravenous Lipid Emulsion During Treatment of Oral Overdoses. Ann Emerg Med. 2015;66:185-8.
Lavonas EJ, Drennan IR, Gabrielli A, Heffner AC, Hoyte CO, Orkin AM, et al. Part 10: Special Circumstances of Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132:S501-18.
Cai Y, Mack A, Ladlie BL, Martin AK. The use of intravenous hydroxocobalamin as a rescue in methylene blue-resistant vasoplegic syndrome in cardiac surgery. Ann Card Anaesth. 2017;20:462-4.
Uhl W, Nolting A, Golor G, Rost KL, Kovar A. Safety of hydroxocobalamin in healthy volunteers in a randomized, placebo-controlled study. Clin Toxicol (Phila). 2006;44 Suppl 1:17-28.
Wong A, Hoffman RS, Walsh SJ, Roberts DM, Gosselin S, Bunchman TE, et al. Extracorporeal treatment for calcium channel blocker poisoning: systematic review and recommendations from the EXTRIP workgroup. Clin Toxicol (Phila). 2021;59:361-75.
Ghannoum M, Hoffman RS, Gosselin S, Nolin TD, Lavergne V, Roberts DM. Use of extracorporeal treatments in the management of poisonings. Kidney Int. 2018;94:682-8.
Masson R, Colas V, Parienti JJ, Lehoux P, Massetti M, Charbonneau P, et al. A comparison of survival with and without extracorporeal life support treatment for severe poisoning due to drug intoxication. Resuscitation. 2012;83:1413-7.
Wang AL, Iadecola C, Wang G. New generations of dihydropyridines for treatment of hypertension. J Geriatr Cardiol. 2017;14:67-72.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




