The One-Year Results of Endovascular Aneurysm Repair for Infrarenal Abdominal Aortic Aneurysm in Rajavithi Hospital
Keywords:
Endovascular aneurysm repair, Abdominal aortic aneurysm, EVAR, EndoleakAbstract
Objectives: To study the one-year results of EVAR for infrarenal AAA patients in Rajavithi Hospital.
Methods: This study conducted a retrospective chart review of all patients with infrarenal AAA who underwent EVAR between January 2017 and February 2021. Medical records were analyzed for demographic data, anatomic features of AAA, procedural details, and 30-day and 1-year outcomes. The primary outcomes were technical success and clinical success at one-year follow-up. Secondary outcomes included perioperative complications, mortality, stent-graft-related complications, and secondary interventions.
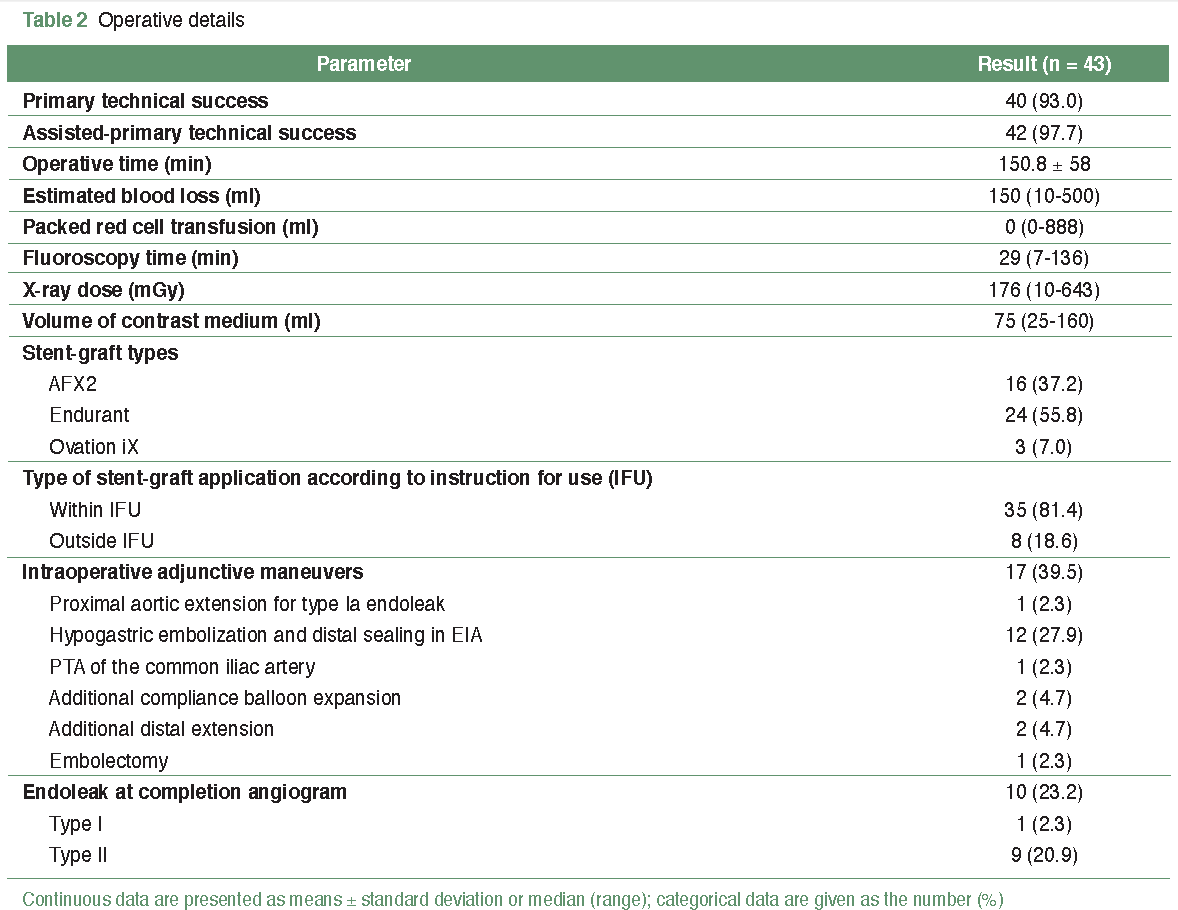
Results: This study included 43 patients (32 men) with a mean age of 72 ± 8.4 years. Successful primary technical success was achieved in 40 patients (93%). The mean operative time was 150.8 ± 58 min, and the median estimated blood loss was 150 ml. The median hospital stay was eight days. Major complications occurred in 9 (20.9%) patients, including 1 myocardial infarction, 1 congestive heart failure, 2 cardiac arrhythmias, 3 pneumonia-related respiratory failures, 2 ischemic colitis, and 2 renal failures requiring hemodialysis. The 30-day mortality was 4.7% (2 patients; one with infected AAA with aortoenteric fistula, and one with pneumonia and multisystem organ failure. A 1-year overall mortality was 16.3%, and AAA-related mortality was 2.3%. A 1-year clinical success rate of 91.4% was observed in 32 out of 35 patients. No cases of stent-graft thrombosis, stent-graft infection, ruptured AAA, open conversion, or type III or IV endoleak were documented in the study.
Conclusion: EVAR can be successfully performed at Rajavithi Hospital with high success and low AAA-related mortality rate. However, it is crucial to emphasize the importance of surveillance to promptly detect and effectively treat any potential complications that may arise.
References
Golledge J, Muller J, Daugherty A, et al. Abdominal aortic aneurysm: pathogenesis and implications for management. Arterioscler Thromb Vasc Biol 2006;26:2605-13. doi:10.1161/01.ATV.0000245819.32762.cb.
Ashton HA, Buxton MJ, Day NE, et al. The Multicentre Aneurysm Screening Study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial. Lancet 2002;360:1531-9. doi:10.1016/s0140-6736(02)11522-4.
Lindholt JS, Juul S, Fasting H, et al. Screening for abdominal aortic aneurysms: single centre randomised controlled trial. BMJ. 2005;330:750. doi:10.1136/bmj.38369.620162.82.
Norman PE, Jamrozik K, Lawrence-Brown MM, et al. Population based randomised controlled trial on impact of screening on mortality from abdominal aortic aneurysm. BMJ. 2004;329:1259. doi:10.1136/bmj.38272.478438.55.
Parodi JC, Palmaz JC, Barone HD. Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg 1991;5:491-9. doi:10.1007/BF02015271.
Greenhalgh RM, Brown LC, Kwong GP, et al. Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomised controlled trial. Lancet 2004;364:843-8. doi:10.1016/S0140-6736(04)16979-1.
Prinssen M, Verhoeven EL, Buth J, et al. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med 2004;351:1607-18. doi:10.1056/NEJMoa042002.
Lederle FA, Freischlag JA, Kyriakides TC, et al. Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA 2009;302:1535-42. doi:10.1001/jama.2009.1426.
Becquemin JP, Pillet JC, Lescalie F, et al. A randomized controlled trial of endovascular aneurysm repair versus open surgery for abdominal aortic aneurysms in low- to moderate-risk patients. J Vasc Surg 2011;53:1167-73. doi:10.1016/j.jvs.2010.10.124.
Paravastu SCV, Jayarajasingam R, Cottam R, et al. Endovascular repair of abdominal aortic aneurysm. Cochrane Database Syst Rev. 2014:CD004178. doi:10.1002/14651858.CD004178.pub2.
Chinsakchai K, Phetpoonpipat W, Ruangsetakit C, et al. Outcomes of asymptomatic abdominal aortic aneurysm as compared between open aortic repair and endovascular rneurysm repair. J Med Assoc Thai 2017;100:162.
Tanpornchai J, Pootracool P, Klinsukon T, et al. Early outcomes of endovascular aortic aneurysm repair in difficult anatomy in Thai patients: multicenter study. J Vasc Surg 2018;68:e140. doi:10.1016/j.jvs.2018.08.080.
Chinsakchai K, Hongku K, Hahtapornsawan S, et al. Outcomes of abdominal aortic aneurysm with aortic neck thrombus after endovascular abdominal aortic aneurysm repair. J Med Assoc Thai. 2014;97:518-24.
Chaikof EL, Blankensteijn JD, Harris PL, et al. Reporting standards for endovascular aortic aneurysm repair. J Vasc Surg 2002;35:1048-60. doi:10.1067/mva.2002.123763.
Elkouri S, Gloviczki P, McKusick MA, et al. Endovascular repair of abdominal aortic aneurysms: initial experience with 100 consecutive patients. Mayo Clin Proc. 2003;78:1234-42. doi:10.4065/78.10.1234.
Biebl M, Hakaim AG, Oldenburg WA, et al. Midterm results of a single-center experience with commercially available devices for endovascular aneurysm repair. Mt Sinai J Med. 2005;72:127-35.
van Keulen JW, de Vries JP, Dekker H, et al. One-year multicenter results of 100 abdominal aortic aneurysm patients treated with the Endurant stent graft. J Vasc Surg 2011;54:609-15. doi:10.1016/j.jvs.2011.02.053.
Makaroun MS, Tuchek M, Massop D, et al. One year outcomes of the United States regulatory trial of the Endurant Stent Graft System. J Vasc Surg 2011;54:601-8. doi:10.1016/j.jvs.2011.03.002.
Carpenter JP, Cuff R, Buckley C, et al. One-year pivotal trial outcomes of the Nellix system for endovascular aneurysm sealing. J Vasc Surg 2017;65:330-336.e4. doi:10.1016/j.jvs.2016.09.024.
Herman CR, Charbonneau P, Hongku K, et al. Any nonadherence to instructions for use predicts graft-related adverse events in patients undergoing elective endovascular aneurysm repair. J Vasc Surg 2018;67:126-133. doi:10.1016/j.jvs.2017.05.095.
Janho KE, Rashaideh MA, Shishani J, et al. Outcomes of Elective Endovascular Aneurysmal Repair for Abdominal Aortic Aneurysms in Jordan. Vasc Specialist Int. 2019;35:202-8. doi:10.5758/vsi.2019.35.4.202.
D’Oria M, Mastrorilli D, Ziani B. Natural history, diagnosis, and management of type II endoleaks after endovascular aortic repair: review and update. Ann Vasc Surg 2020;62:420-31. doi:10.1016/j.avsg.2019.04.048.
Samura M, Morikage N, Mizoguchi T, et al. Effectiveness of embolization of inferior mesenteric artery to prevent type II endoleak following endovascular aneurysm repair: a review of the literature. Ann Vasc Dis 2018;11:259-64. doi:10.3400/avd.ra.18-00064.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Royal College of Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles must be contributed solely to The Thai Journal of Surgery and when published become the property of the Royal College of Surgeons of Thailand. The Royal College of Surgeons of Thailand reserves copyright on all published materials and such materials may not be reproduced in any form without the written permission.


