Association of Diaphragmatic Function by Ultrasound and WIND Classification in Surgical Intensive Care Unit
Keywords:
Weaning, Mechanical ventilation, Ultrasound, Diaphragm, Diaphragm dysfunctionAbstract
Background: The issue of weaning patients off mechanical ventilation remains a significant concern within the intensive care unit (ICU). Weaning, as defined by the Weaning according to a New Definition (WIND), is a valuable approach for predicting the probability of successful extubation or potential complications following mechanical ventilation. Ultrasonic diagnostics have emerged as a promising tool for evaluating various aspects of diaphragmatic function.
Objective: To investigate the relationship between ultrasonic diaphragmatic parameters and the WIND classification group.
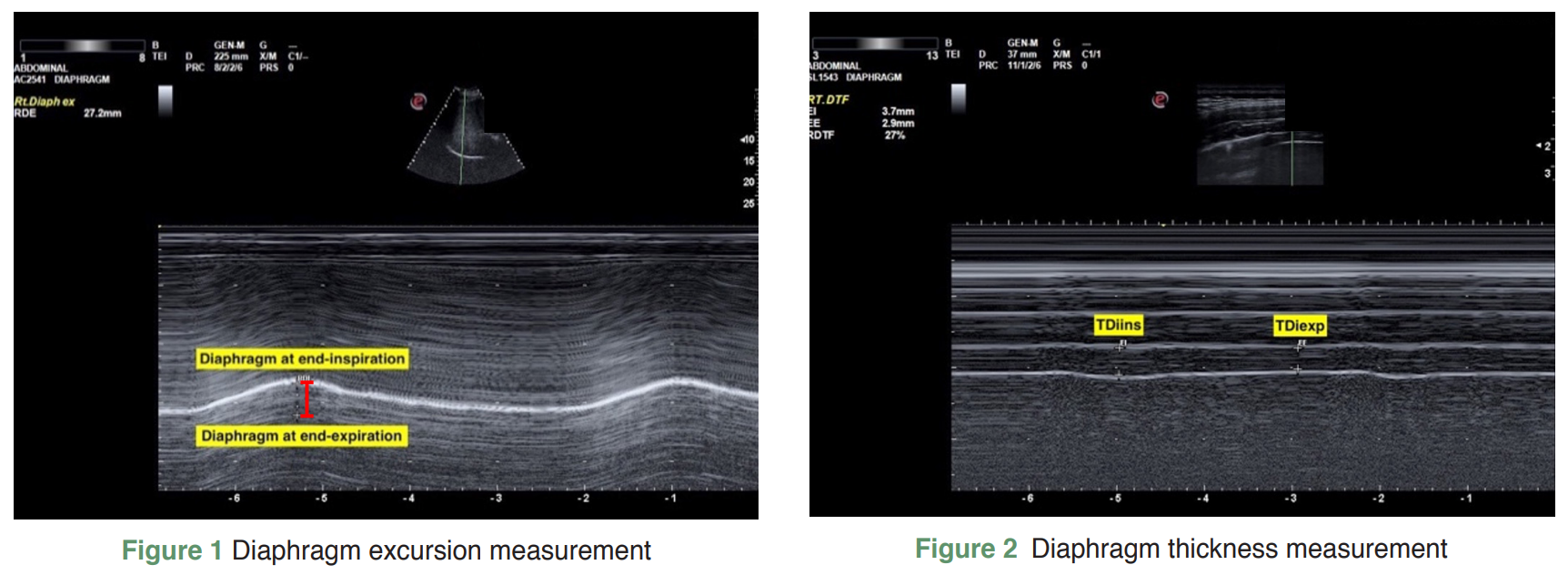
Methods: This was a prospective observational study in which intubated surgical intensive care unit (SICU) patients were included. Diaphragmatic ultrasounds were performed on these patients. After the patients were discharged from the SICU, they were classified into each WIND group, and the association between the WIND group and diaphragmatic ultrasound parameters was analyzed.
Results: A total of 128 mechanically ventilated patients were included in the study. The majority of patients, 90 (70%), were assigned to the WIND 1 group, while 24 (19%) were assigned to the WIND 2 group, and 8 (6%) were assigned to the WIND 3 group. Additionally, 6 (5%) patients were assigned to the WIND NW group. The median age of the patients was 67, with a range of 53 to 75. The most common type of respiratory failure experienced by the patients was peri-operative, accounting for 68% of cases. There were no significant differences observed in other baseline characteristics among the different groups. However, when examining diaphragmatic thickness at the end inspiration, a statistically significant difference was found on the right side. The WIND 3 group had the lowest measurement of diaphragmatic thickness at 1.5 mm. It is important to note that there were no significant differences in diaphragmatic thickness parameters between the groups.
Conclusions: Diaphragmatic ultrasonography lacks the ability to differentiate between the various WIND groups. However, the success of weaning is different among WIND classifications.
References
Chittawatanarat K, Chaiwat O, Morakul S, et al. A multi-center Thai university - based surgical intensive care units study (THAI-SICU study): Methodology and ICU characteristics. J Med Assoc Thai. 2014;97:S45-S54.
Chaiwat O, Chittawatanarat K, Piriyapathsom A, et al. Incidence of and risk factors for acute respiratory distress syndrome in patients admitted to surgical intensive care units: the multicenter Thai University-based surgical intensive care unit (THAI-SICU Study). J Med Assoc Thai 2016;99:S118-27.
Chittawatanarat K, Orrapin S, Jitkaroon K, et al. An Open Label Randomized Controlled Trial to Compare Low Level Pressure Support and T-piece as Strategies for Discontinuation of Mechanical Ventilation in a General Surgical Intensive Care Unit. Med Arch. 2018;72:51-7. doi:10.5455/medarh.2018.72.51-57.
Chittawatanarat K, Thongchai C. Spontaneous breathing trial with low pressure support protocol for weaning respirator in surgical ICU. J Med Assoc Thai. 2009;92:1306-12.
Gao F, Yang LH, He HR, et al. The effect of reintubation on ventilator-associated pneumonia and mortality among mechanically ventilated patients with intubation: A systematic review and meta-analysis. Heart Lung. 2016;45:363-71. doi:10.1016/j.hrtlng.2016.04.006.
Jeong BH, Lee KY, Nam J, et al. Validation of a new WIND classification compared to ICC classification for weaning outcome. Ann Intensive Care. 2018;8:115. doi:10.1186/s13613-018-0461-z.
Beduneau G, Pham T, Schortgen F, et al. Epidemiology of Weaning Outcome according to a New Definition. The WIND Study. Am J Respir Crit Care Med. 2017;195:772-83. doi:10.1164/rccm.201602-0320OC.
Kulkanokwan N, Morakul S, Pisitsak C, et al. Comparison of ultrasound assessment for diaphragmatic workload during spontaneous breathing trial between automatic tube compensation and pressure support ventilation: Study protocol. Clin Crit Care. 2022;30:2022:e0004.
Ferrari G, De Filippi G, Elia F, et al. Diaphragm ultrasound as a new index of discontinuation from mechanical ventilation. Crit Ultrasound J. 2014;6:8. doi:10.1186/2036-7902-6-8.
Dres M, Goligher EC, Dube BP, et al. Diaphragm function and weaning from mechanical ventilation: an ultrasound and phrenic nerve stimulation clinical study. Ann Intensive Care. 2018;8:53. doi:10.1186/s13613-018-0401-y.
Somboonviboon D, Oerareemitr N, Wacharasint P. Evaluation of weaning parameters for weaning readiness from mechanical ventilation among elderly patients. Clin Crit Care. 2022;30:2022:e0017.
Zambon M, Greco M, Bocchino S, et al. Assessment of diaphragmatic dysfunction in the critically ill patient with ultrasound: a systematic review. Intensive Care Med. 2017;43:29-38. doi:10.1007/s00134-016-4524-z.
Ali ER, Mohamad AM. Diaphragm ultrasound as a new functional and morphological index of outcome, prognosis and discontinuation from mechanical ventilation in critically ill patients and evaluating the possible protective indices against VIDD. Egypt J Chest Dis Tubercu. 2017;66:339-51. doi:10.1016/j.ejcdt.2016.10.006.
Umbrello M, Formenti P. Ultrasonographic Assessment of Diaphragm Function in Critically Ill Subjects. Respir Care. 2016;61:542-55. doi:10.4187/respcare.04412.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Royal College of Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles must be contributed solely to The Thai Journal of Surgery and when published become the property of the Royal College of Surgeons of Thailand. The Royal College of Surgeons of Thailand reserves copyright on all published materials and such materials may not be reproduced in any form without the written permission.


