Survival and Treatment Outcomes of Resectable Cholangiocarcinoma: Initial Experience in Khon Kaen Hospital
Keywords:
Cholangiocarcinoma surgeryAbstract
Background: The most effective current treatment for cholangiocarcinoma is surgical resection. Khon Kaen Hospital receives a significant number of cholangiocarcinoma patients, and it is essential to analyze the treatment outcomes and survival to improve future treatment processes.
Methods: A retrospective study that analyzes the treatment outcomes and survival of cholangiocarcinoma patients who underwent surgery at Khon Kaen Hospital between October 2014 to September 2019. The study covers patient demographics, disease characteristics, surgical information, treatment outcomes, complications, and survival analysis.
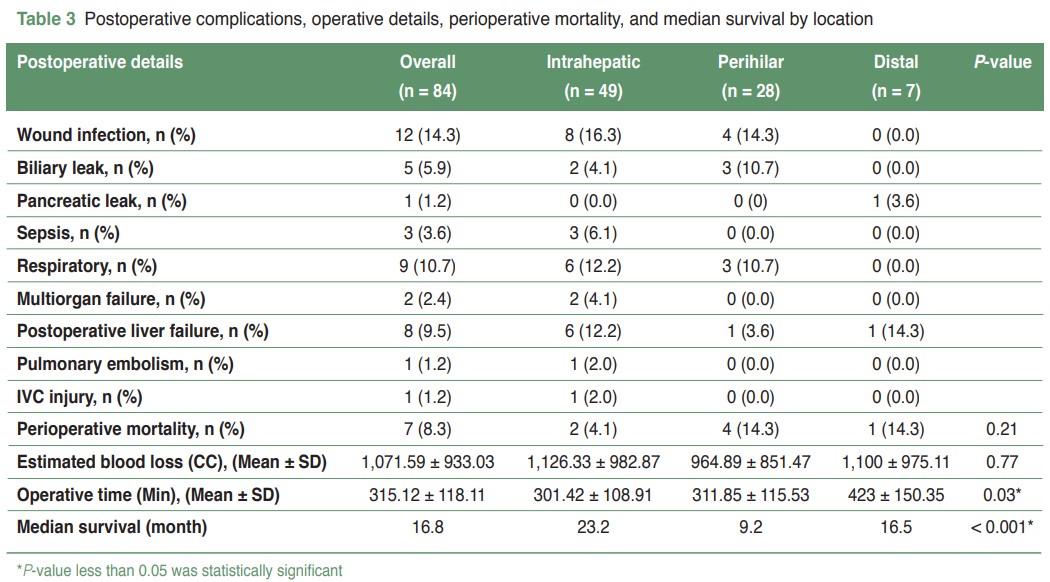
Results: There were a total of 84 predominantly male patients with an average age of 63 years. Most patients had intrahepatic type and presented with abdominal pain and jaundice. The most common complication was wound infection, 14%, and the overall perioperative mortality rate was 8%. The perihilar type had the highest mortality rate. The median survival time was 16.8 months, with the intrahepatic type having the most prolonged survival (23.2 months), followed by distal type (16.5 months) and perihilar type (9.2 months). These differences were statistically significant (P-value < 0.01). Positive margins and lymph node involvement were significant factors associated with shorter survival times.
Conclusion: Surgical treatment of cholangiocarcinoma at Khon Kaen Hospital is generally safe, with complication and mortality rates comparable to other research studies. Key factors for long-term survival include achieving a negative microscopic margin (R0 resection) and the absence of lymph node involvement.
References
Green A, Uttaravichien T, Bhudhisawasdi V, et al. Cholangiocarcinoma in north east Thailand. A hospital-based study. Trop Geogr Med. 1991;43(1-2):193-8.
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Infection with liver flukes (Opisthorchis viverrini, Opisthorchis felineus and Clonorchis sinensis). IIARC Monograph on the Evaluation of Carcinogenic Risks to Humans. Lyon (FR): IARC. 1994;61:121-75.
Nakeeb A, Pitt HA, Sohn TA, et al. Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg. 1996;224(4):463-73; discussion 473-5. doi: 10.1097/00000658-199610000-00005.
Mihalache F, Tantau M, Diaconu B, et al. Survival and quality of life of cholangiocarcinoma patients: a prospective study over a 4 year period. J Gastrointestin Liver Dis. 2010;19(3):285-90.
Witzigmann H, Berr F, Ringel U, et al. Surgical and palliative management and outcome in 184 patients with hilar cholangiocarcinoma: palliative photodynamic therapy plus stenting is comparable to r1/r2 resection. Ann Surg. 2006;244(2):230-9. doi: 10.1097/01.sla.0000217639.10331.47.
Reding R, Buard JL, Lebeau G, et al. Surgical management of 552 carcinomas of the extrahepatic bile ducts (gallbladder and periampullary tumors excluded). Results of the French Surgical Association Survey. Ann Surg. 1991;213(3):236-41. doi: 10.1097/00000658-199103000-00010.
Aljiffry M, Abdulelah A, Walsh M, et al. Evidence-based approach to cholangiocarcinoma: a systematic review of the current literature. J Am Coll Surg. 2009;208(1):134-47. doi: 10.1016/j.jamcollsurg.2008.09.007.
Henson DE, Albores-Saavedra J, Corle D. Carcinoma of the extrahepatic bile ducts. Histologic types, stage of disease, grade, and survival rates. Cancer. 1992;70(6):1498-501. doi: 10.1002/1097-0142(19920915)70:6<1498::aid-cncr2820700609>3.0.co;2-c.
Henson DE, Albores-Saavedra J, Corle D. Carcinoma of the gallbladder. Histologic types, stage of disease, grade, and survival rates. Cancer. 1992;70(6):1493-7. doi: 10.1002/1097-0142(19920915)70:6<1493::aid-cncr2820700608>3.0.co;2-u.
Iwatsuki S, Todo S, Marsh JW, et al. Treatment of hilar cholangiocarcinoma (Klatskin tumors) with hepatic resection or transplantation. J Am Coll Surg. 1998;187(4):358-64. doi: 10.1016/s1072-7515(98)00207-5.
Otto G, Hoppe-Lotichius M, Bittinger F, et al. Klatskin tumour: meticulous preoperative work-up and resection rate. Z Gastroenterol. 2011;49(4):436-42. doi: 10.1055/s-0029-1246011.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Royal College of Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles must be contributed solely to The Thai Journal of Surgery and when published become the property of the Royal College of Surgeons of Thailand. The Royal College of Surgeons of Thailand reserves copyright on all published materials and such materials may not be reproduced in any form without the written permission.


