Decoding Factors Influencing Post-Operative Outcomes in Surgical Residents' Minor Surgeries
Keywords:
Minor surgery, Complication, Surgical resident, TrainingAbstract
Objective: Effective surgical residency training is essential for developing competent surgeons. The first year of training focuses on basic knowledge and fundamental surgical skills. Consequently, minor surgical procedures suit first-year surgical residents with minimal complexity and low complication rates. This pilot study aimed to evaluate the complications associated with surgical residency practice and examine the factors associated with these complications.
Materials and Methods: This study employed a single-center retrospective review method to evaluate the complications arising from surgical residents' minor operations and identify the factors associated with these complications. Data were collected at Siriraj Hospital over three consecutive years, from 2016 to 2018.
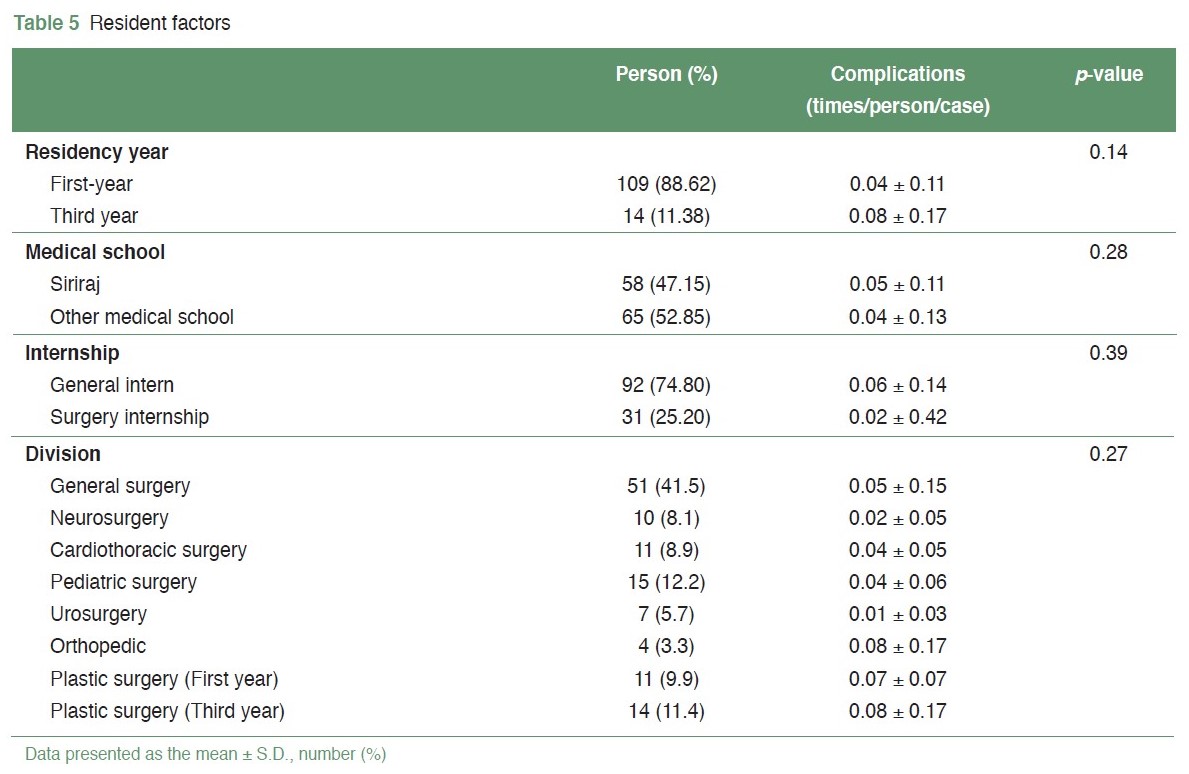
Results: During the study period, a total of 1,572 minor operations were performed by surgical residents. The overall complication rate was 4.3%, which included surgical site infections, wound dehiscence, hematoma or bleeding, seroma, and superficial skin necrosis. Among the surgical site infection cases, an operative time exceeding 30 minutes (OR 13.3, p-value = 0.00) and lesion size larger than two centimeters (OR 5.24, p-value = 0.01) were significant influencing factors for complications. Conversely, residents' background characteristics and the presence of a 'July effect' did not significantly impact surgical outcomes.
Conclusion: The rate of complications associated with minor operations performed by residents at Siriraj Hospital was comparable to the findings from other studies. The most common complications were wound dehiscence and surgical site infections. Operative time and lesion size were significant factors affecting complications. The results of this study can contribute to enhancing surgical residency training.
References
Wojcik BM, Fong ZV, Patel MS, et al. The Resident-Run Minor Surgery Clinic: A Pilot Study to Safely Increase Operative Autonomy. J Surg Educ. 2016;73(6):e142-e149. doi: 10.1016/j.jsurg.2016.08.016.
Amici JM, Rogues AM, Lasheras A, et al. A prospective study of the incidence of complications associated with dermatological surgery. Br J Dermatol. 2005;153(5):967-71. doi: 10.1111/j.1365-2133.2005.06861.x.
Cheng H, Chen BP, Soleas IM, et al. Prolonged Operative Duration Increases Risk of Surgical Site Infections: A Systematic Review. Surg Infect (Larchmt). 2017;18(6):722-35. doi: 10.1089/sur.2017.089.
van der Leeuw RM, Lombarts KM, Arah OA, et al. A systematic review of the effects of residency training on patient outcomes. BMC Med. 2012;10:65. doi: 10.1186/1741-7015-10-65.
Macki M, Fakih M, Rubinfeld I, et al. The Impact of Different Postgraduate Year Training in Neurosurgery Residency on 30-Day Postoperative Outcomes. Neurosurgery. 2019;84(3):778-87. doi: 10.1093/neuros/nyy277.
Worley P, Esterman A, Prideaux D. Cohort study of examination performance of undergraduate medical students learning in community settings. BMJ. 2004;328(7433):207-9. doi: 10.1136/bmj.328.7433.207.
Asch DA, Nicholson S, Srinivas S, et al. Evaluating obstetrical residency programs using patient outcomes. JAMA. 2009;302(12):1277-83. doi: 10.1001/jama.2009.1356.
Young JQ, Ranji SR, Wachter RM, et al. "July effect": impact of the academic year-end changeover on patient outcomes: a systematic review. Ann Intern Med. 2011;155(5):309-15. doi: 10.7326/0003-4819-155-5-201109060-00354.
Blough JT, Jordan SW, De Oliveira GS, et al. Demystifying the “July Effect” in Plastic Surgery: A Multi-Institutional Study. Aesthet Surg J. 2018;38(2):212–24. doi: 10.1093/asj/sjx099.
American Board of Surgery. Booklet of Information - Surgery; 2023-2024. [cited 2022 April 2]. Available from: https://www.absurgery.org/xfer/BookletofInfo-Surgery.pdf.
Surgical Council on Resident Education. SCORE Curriculum Outline; 2009-2024. [cited 2022 April 2]. Available from: https://www.surgicalcore.org/public/curriculum#gensurg.
The Royal College of Surgeons of Thailand. Residency Training in Surgery curriculum; 2015. [cited 2022 April 2]. Available from: https://www.rcst.or.th/th/training-courses/.
Chan E, Bucevska M, Verchere C. Minor surgery procedures: A retrospective review and prospective survey in a pediatric population. Plast Surg (Oakv). 2015;23(3):189-94. doi: 10.4172/plastic-surgery.1000929.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309-32. doi: 10.1016/j.ajic.2008.03.002.
Li K, Sambare TD, Jiang SY, et al. Effectiveness of Preoperative Antibiotics in Preventing Surgical Site Infection After Common Soft Tissue Procedures of the Hand. Clin Orthop Relat Res. 2018;476(4):664-73. doi: 10.1007/s11999.0000000000000073.
Liu X, Sprengers M, Nelemans PJ, et al. Risk Factors for Surgical Site Infections in Dermatological Surgery. Acta Derm Venereol. 2018;98(2):246-50. doi: 10.2340/00015555-2844.
Kulichová D, Geimer T, Mühlstädt M, et al. Surgical site infections in skin surgery: a single center experience. J Dermatol. 2013;40(10):779-85. doi: 10.1111/1346-8138.12255.
Sandy-Hodgetts K, Carville K, Leslie GD. Determining risk factors for surgical wound dehiscence: a literature review. Int Wound J. 2015;12(3):265-75. doi: 10.1111/iwj.12088.
Seyffert J, Harding T, Sanghvi A, et al. Surgical Wound Dehiscence Following Cutaneous Excisions: A Retrospective Study and Review of the Literature. JDDS. 2020;24(2):93-8. Doi: 10.4103/jdds.jdds_71_20.
Campbell RM, Dufresne RG. Dehiscence and necrosis. In: Gloster HM, ed. Complications in Cutaneous Surgery. New York: Springer, 2008:80.
Iglesias Zamora ME, Aróstegui Aguilar J. Safety in Dermatologic Procedures: How to Prevent, Recognize, and Treat Bleeding Complications in Dermatologic Surgery. Actas Dermosifiliogr. 2022;113(1):67-71. English, Spanish. doi: 10.1016/j.ad.2021.05.014.
Bunick CG, Aasi SZ. Hemorrhagic complications in dermatologic surgery. Dermatol Ther. 2011;24(6):537-50. doi: 10.1111/j.1529-8019.2012.01454.x.
Koenen W, Kunte C, Hartmann D, et al. Prospective multicentre cohort study on 9154 surgical procedures to assess the risk of postoperative bleeding - a DESSI study. J Eur Acad Dermatol Venereol. 2017;31(4):724-31. doi: 10.1111/jdv.14080.
Iyengar S, Yeager DG, Cohen JL, et al. Update and Review of Bleeding Considerations in Dermatologic Surgery: Hemostatic Techniques and Treatment Strategies for Bleeding Complications. Dermatol Surg. 2020;46(2):203-12. doi: 10.1097/DSS.0000000000002138.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The Royal College of Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles must be contributed solely to The Thai Journal of Surgery and when published become the property of the Royal College of Surgeons of Thailand. The Royal College of Surgeons of Thailand reserves copyright on all published materials and such materials may not be reproduced in any form without the written permission.


