Clinical Outcomes Following Surgical Revascularization for Acute Lower Limb Ischemia
Keywords:
Acute lower limb ischemia (ALI), Embolism, Thrombosis, Revascularization, Limb salvageAbstract
Objectives: To assess the clinical outcomes of surgical revascularization in patients diagnosed with acute lower limb ischemia (ALI). The primary outcome was defined as the limb salvage rate within 30 days after surgery.
Methods: This is a retrospective single-center study. The target population was recruited from the Prapokklao Hospital database between January 2019 – December 2023. Patients who were diagnosed with acute occlusion of the artery according to the International Classification of Disease 10th Revision (ICD-10) code I74.0, I74.3, and I74.5 were identified. Medical records were analyzed for demography, clinical presentation, etiology, Rutherford severity classification, revascularization procedures, major amputation, mortality within 30 days after revascularization, and data during follow-up.
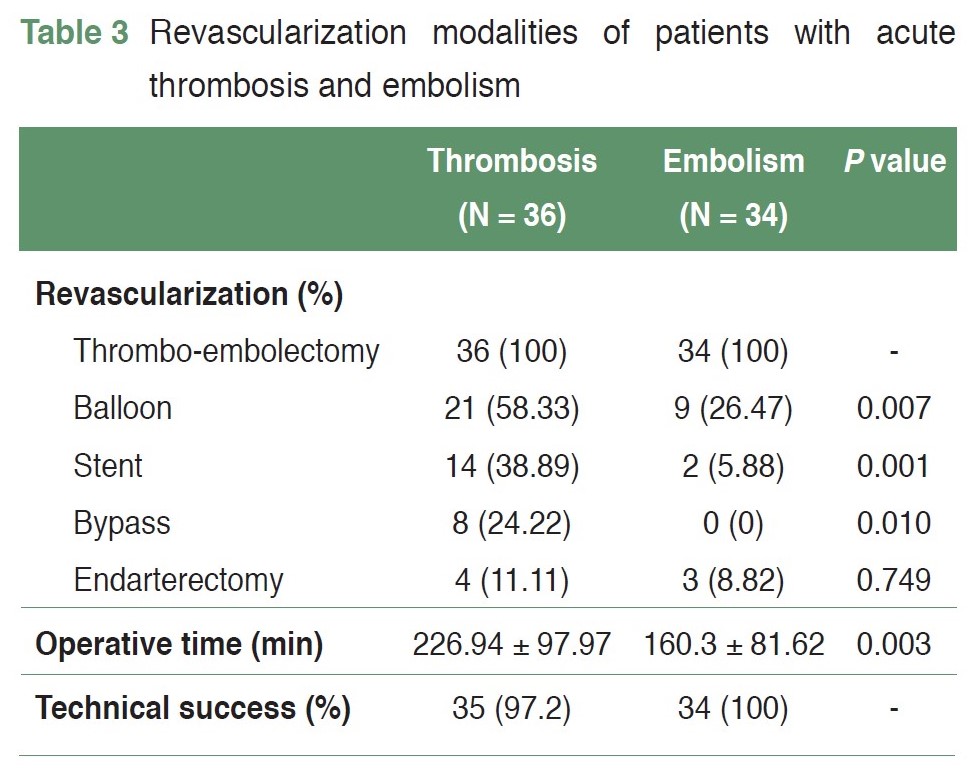
Results: This study enrolled a total of 70 patients, 46 men (65.71%) and 77 affected limbs. The mean age was 65.67 years (SD 13.69 years), and the median was 65 years, ranging from 19 to 94 years. Co-morbidities: 42 (60%) hypertension, 28 (40%) peripheral arterial disease, 26 (37.14%) atrial fibrillation. Etiologies: 36 (51.43%) thrombosis (34.29% in-situ thrombosis of the native vessel) and 34 (48.57%) embolism. Rutherford classification of severity categories I, IIa, and IIb was 1 (1.42%), 21 (30.0%), and 48 (68.58%), respectively. The modalities of revascularization included 70 (100 %) thromboembolectomy with a Fogarty catheter, 30 (42.86%) intra-arterial angioplasty with balloon or stent, 8 (11.43%) bypass procedure, 6 (8.57%) endarterectomy and 8 (11.42%) fasciotomy. Technical success was 98.57 %. The mean operative time was 195.07 minutes (SD 95.51 minutes). The median hospital stay was 8 days. Post-operative complications were 8 (11.43%) bleeding, 7 (10%) compartment syndrome, 5 (7.14%) reperfusion injury, 5 (7.14%) acute kidney injury, 2 (2.86%) pneumonia and 1 (1.43%) acute myocardial infarction. The 30-day major amputation rate and mortality were 10.0% and 5.71%, respectively. At 30 days, sixty-three patients (90%) had limb salvage, and Four (5.71%) patients had died.
Conclusion: Clinical outcomes following surgical revascularization for acute lower limb ischemia in our hospital showed high technical success and limb salvage rates. The limb salvage rate was 90.0%, and the mortality rate was 5.71%.
References
Norgren L, Hiatt WR, Dormandy JA, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg. 2007;33(Suppl 1):S1-75. doi: 10.1016/j.ejvs.2006.09.024.
Jonothan JE. Acute Limb Ischemia: Evaluation, Decision Making. In: Cronenwett JL, Johnston KW. Rutherford's Vascular Surgery, Eighth Edition, Volume 1. Philadelphia: Elsevier/Saunders, 2014:2518-26.
Creager MA, Kaufman JA, Conte MS. Clinical practice. Acute limb ischemia. N Engl J Med. 2012;366(23):2198-206. doi: 10.1056/NEJMcp1006054.
Rutherford RB, Baker JD, Ernst C, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997;26(3):517-38. doi: 10.1016/s0741-5214(97)70045-4.
Björck M, Earnshaw JJ, Acosta S, et al. Editor's Choice - European Society for Vascular Surgery (ESVS) 2020 Clinical Practice Guidelines on the Management of Acute Limb Ischaemia. Eur J Vasc Endovasc Surg. 2020;59(2):173-218. doi: 10.1016/j.ejvs.2019.09.006.
Mutirangura P, Ruangsetakit C, Wongwanit C, et al. Acute arterial embolism of the lower extremities: impact of 24-hour duration on the outcome of management. J Med Assoc Thai. 2008;91(9):1360-7.
Umetsu M, Akamatsu D, Goto H, et al. Long-Term Outcomes of Acute Limb Ischemia: A Retrospective Analysis of 93 Consecutive Limbs. Ann Vasc Dis. 2019;12(3):347-53. doi: 10.3400/avd.oa.19-00018.
Kulezic A, Acosta S. Epidemiology and Prognostic Factors in Acute Lower Limb Ischaemia: A Population Based Study. Eur J Vasc Endovasc Surg. 2022;63(2):296-303. doi: 10.1016/j.ejvs.2021.10.044.
Baril DT, Patel VI, Judelson DR, et al. Outcomes of lower extremity bypass performed for acute limb ischemia. J Vasc Surg. 2013;58(4):949-56. doi: 10.1016/j.jvs.2013.04.036.
Mutirangura P, Ruangsetakit C, Wongwanit C, et al. Clinical differentiation between acute arterial embolism and acute arterial thrombosis of the lower extremities. J Med Assoc Thai. 2009;92(7):891-7.
Kempe K, Starr B, Stafford JM, et al. Results of surgical management of acute thromboembolic lower extremity ischemia. J Vasc Surg. 2014;60(3):702-7. doi: 10.1016/j.jvs.2014.03.273.
Hill SL, Donato AT. The simple Fogarty embolectomy: an operation of the past? Am Surg. 1994;60(12):907-11.
Bath J, Kim RJ, Dombrovskiy VY, et al. Contemporary trends and outcomes of thrombolytic therapy for acute lower extremity ischemia. Vascular. 2019;27(1):71-7. doi: 10.1177/1708538118797782.
Berczi V, Thomas SM, Turner DR, et al. Stent implantation for acute iliac artery occlusions: initial experience. J Vasc Interv Radiol. 2006;17(4):645-9. doi: 10.1097/01.RVI.0000203918.91835.73.
Kim C, Jeon W, Shin T, et al. Stent-assisted recanalisation of acute occlusive arteries in patients with acute limb ischaemia. Eur J Vasc Endovasc Surg. 2010;39(1):89-96. doi: 10.1016/j.ejvs.2009.09.023.
Hemingway J, Emanuels D, Aarabi S, et al. Safety of transfer, type of procedure, and factors predictive of limb salvage in a modern series of acute limb ischemia. J Vasc Surg. 2019;69(4):1174-9. doi: 10.1016/j.jvs.2018.08.174.
Aune S, Trippestad A. Operative mortality and long-term survival of patients operated on for acute lower limb ischaemia. Eur J Vasc Endovasc Surg. 1998;15(2):143-6. doi: 10.1016/s1078-5884(98)80135-4.
Ljungman C, Holmberg L, Bergqvist D, et al. Amputation risk and survival after embolectomy for acute arterial ischaemia. Time trends in a defined Swedish population. Eur J Vasc Endovasc Surg. 1996;11(2):176-82. doi: 10.1016/s1078-5884(96)80048-7.
Eliason JL, Wainess RM, Proctor MC, et al. A national and single institutional experience in the contemporary treatment of acute lower extremity ischemia. Ann Surg. 2003;238(3):382-9. doi: 10.1097/01.sla.0000086663.49670.d1.
Vakhitov D, Hakovirta H, Saarinen E, et al. Prognostic risk factors for recurrent acute lower limb ischemia in patients treated with intra-arterial thrombolysis. J Vasc Surg. 2020;71(4):1268-75. doi: 10.1016/j.jvs.2019.07.061.
Aboyans V, Ricco JB, Bartelink MEL, et al. Editor's Choice - 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg. 2018;55(3):305-68. doi: 10.1016/j.ejvs.2017.07.018.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The Royal College of Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles must be contributed solely to The Thai Journal of Surgery and when published become the property of the Royal College of Surgeons of Thailand. The Royal College of Surgeons of Thailand reserves copyright on all published materials and such materials may not be reproduced in any form without the written permission.


