Comparison of Mesh Fixation and Non-fixation in Totally Extraperitoneal Hernia Repair: A Randomized Controlled Trial
Keywords:
Laparoscopic inguinal hernia repair, TEP, The EHS groin hernia classification, Mesh fixation, Non-fixationAbstract
Objective: Many studies have shown that non-fixation of mesh in laparoscopic totally extraperitoneal (TEP) inguinal hernia repair is safe and has no disadvantage compared to mesh fixation; however, most studies contain limited information on hernia-defect size. The purpose of this study was to compare the clinical outcome of non-fixation and fixation of mesh in consecutive elective laparoscopic TEP inguinal hernia repair in any type and size of hernia defect classified by the European Hernia Society (EHS) groin hernia classification to be a part of the level 1 evidence about technique of fixation in TEP.
Patients and Methods: One hundred and ten hernia repairs in 101 patients were enrolled in the trial between July 2022 and August 2023. The patients were randomized to the mesh fixation group (n = 55) or the non-fixation group (n = 55). The primary outcomes were chronic groin pain and recurrence at 6 months. The secondary outcomes were operative time, conversion rates, pain scores, analgesic requirement, time to regular activity, complications, and length of stay. A person blinded to the method of fixation performed statistical analysis.
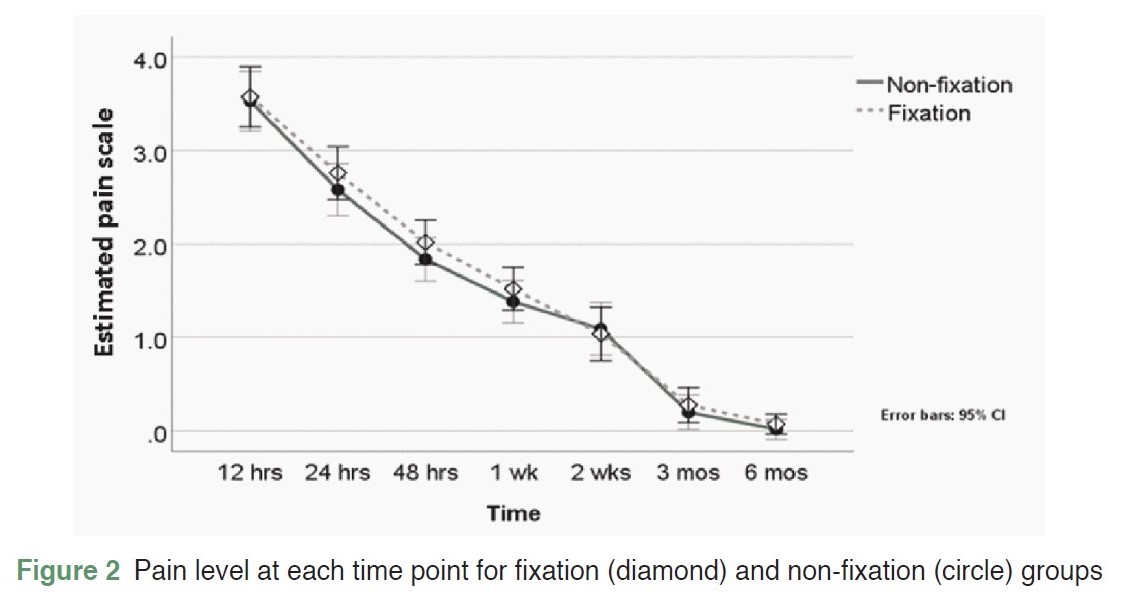
Results: There were no significant differences between the two groups in baseline demographic characteristics, including age, BMI, sex, ASA classification, EHS hernia classification, and incidence of recurrent defect. More than 90% of hernia defects were larger than 1.5 cm, and more than 25% of defects were > 3 cm. They were statistically similar in both groups in terms of chronic groin pain, operative time, conversion rates, pain scores, analgesic requirement, time to regular activity, length of stay, and complications. Neither group had a recurrence at a minimum follow-up of 6 months.
Conclusions: There was no statistical significance in chronic groin pain and recurrence between fixation and non-fixation groups. The non-fixation approach should be adopted routinely and safely in laparoscopic TEP hernia repair. Even the tack fixation technique applied in this study was not associated with the risk of significant pain level and chronic groin pain; however, it is associated with high operative cost, so it should be used only in very selected situations in TEP.
References
Bittner R, Montgomery MA, Arregui E, et al. Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society). Surg Endosc. 2015;29(2):289-321. doi: 10.1007/s00464-014-3917-8.
Martínez-Hoed J, Cordero-Bermúdez K, García-Pastor P, et al. The inguinal hernia management in Costa Rica according to a survey between surgeons: result comparison with 2018 International Groin Hernia Guidelines. BMC Surg. 2021;21(1):152. doi: 10.1186/s12893-021-01156-9.
van Veenendaal N, Simons MP, Bonjer HJ. Summary for patients: International guidelines for groin hernia management. Hernia. 2018;22(1):167-8. doi: https://doi.org/10.1007/s10029-018-1729-9.
McCormack K, Scott NW, Go PM, et al. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2003;2003(1):CD001785. doi: 10.1002/14651858.CD001785.
Chowbey PK, Bandyopadhyay SK, Sharma A, et al. Recurrent hernia following endoscopic total extraperitoneal repair. J Laparoendosc Adv Surg Tech A. 2003;13(1):21-5. doi: 10.1089/109264203321235421.
Ferzli GS, Frezza EE, Pecoraro AM Jr, et al. Prospective randomized study of stapled versus unstapled mesh in a laparoscopic preperitoneal inguinal hernia repair. J Am Coll Surg. 1999;188(5):461-5. doi: 10.1016/s1072-7515(99)00039-3.
Kobayashi F, Watanabe J, Koizumi M, et al. Efficacy and safety of mesh non-fixation in patients undergoing laparo-endoscopic repair of groin hernia: a systematic review and meta-analysis. Hernia. 2023;27(6):1415-27. doi: 10.1007/s10029-023-02919-4.
Moreno-Egea A, Torralba Martínez JA, Morales Cuenca G, et al. Randomized clinical trial of fixation vs nonfixation of mesh in total extraperitoneal inguinal hernioplasty. Arch Surg. 2004;139(12):1376-9. doi: 10.1001/archsurg.139.12.1376.
Taylor C, Layani L, Liew V, et al. Laparoscopic inguinal hernia repair without mesh fixation, early results of a large randomised clinical trial. Surg Endosc. 2008;22(3):757-62. doi: 10.1007/s00464-007-9510-7.
Daes J, Felix E. Critical View of the Myopectineal Orifice. Ann Surg. 2017;266(1):e1-e2. doi: 10.1097/SLA.0000000000002104.
Miserez M, Alexandre JH, Campanelli G, et al. The European hernia society groin hernia classification: simple and easy to remember. Hernia. 2007;11(2):113-6. doi: 10.1007/s10029-007-0198-3.
Usmani F, Wijerathne S, Malik S, et al. Effect of direct defect closure during laparoscopic inguinal hernia repair ("TEP/TAPP plus" technique) on post-operative outcomes. Hernia. 2020;24(1):167-71. doi: 10.1007/s10029-019-02036-1.
Ng AY, Lin J, Ching SS, et al. Does primary closure of direct inguinal hernia defect during laparoscopic mesh repair reduce the risk of early recurrence? Hernia. 2020;24(5):1093-8. doi: 10.1007/s10029-020-02257-9.
Li W, Li Y, Ding L, et al. A randomized study on laparoscopic total extraperitoneal inguinal hernia repair with hernia sac transection vs complete sac reduction. Surg Endosc. 2020;34(4):1882-6. doi: 10.1007/s00464-019-07303-x.
Claus C, Furtado M, Malcher F, et al. Ten golden rules for a safe MIS inguinal hernia repair using a new anatomical concept as a guide. Surg Endosc. 2020;34(4):1458-64. doi: 10.1007/s00464-020-07449-z.
Garg P, Nair S, Shereef M, et al. Mesh fixation compared to nonfixation in total extraperitoneal inguinal hernia repair: a randomized controlled trial in a rural center in India. Surg Endosc. 2011;25(10):3300-6. doi: 10.1007/s00464-011-1708-z.
Burati M, Scaini A, Fumagalli LA, et al. Mesh Fixation Methods in Groin Hernia Surgery. In: Guttadauro A. Techniques and Innovation in Hernia Surgery. Rijeka: IntechOpen, 2019. doi: 10.5772/intechopen.89732.
Garg P, Rajagopal M, Varghese V, et al. Laparoscopic total extraperitoneal inguinal hernia repair with nonfixation of the mesh for 1,692 hernias. Surg Endosc. 2009;23(6):1241-5. doi: 10.1007/s00464-008-0137-0.
Ismail M, Garg P. Laparoscopic inguinal total extraperitoneal hernia repair under spinal anesthesia without mesh fixation in 1,220 hernia repairs. Hernia. 2009;13(2):115-9. doi: 10.1007/s10029-008-0442-5.
Sajid MS, Ladwa N, Kalra L, et al. A meta-analysis examining the use of tacker fixation versus no-fixation of mesh in laparoscopic inguinal hernia repair. Int J Surg. 2012;10(5):224-31. doi: 10.1016/j.ijsu.2012.03.001.
Teng YJ, Pan SM, Liu YL, et al. A meta-analysis of randomized controlled trials of fixation versus nonfixation of mesh in laparoscopic total extraperitoneal inguinal hernia repair. Surg Endosc. 2011;25(9):2849-58. doi: 10.1007/s00464-011-1668-3.
Tam KW, Liang HH, Chai CY. Outcomes of staple fixation of mesh versus nonfixation in laparoscopic total extraperitoneal inguinal repair: a meta-analysis of randomized controlled trials. World J Surg. 2010;34(12):3065-74. doi: 10.1007/s00268-010-0760-5.
Choy C, Shapiro K, Patel S, et al. Investigating a possible cause of mesh migration during totally extraperitoneal (TEP) repair. Surg Endosc. 2004;18(3):523-5. doi: 10.1007/s00464-003-8183-0.
Khajanchee YS, Urbach DR, Swanstrom LL, et al. Outcomes of laparoscopic herniorrhaphy without fixation of mesh to the abdominal wall. Surg Endosc. 2001;15(10):1102-7. doi: 10.1007/s004640080088.
Beattie GC, Kumar S, Nixon SJ. Laparoscopic total extraperitoneal hernia repair: mesh fixation is unnecessary. J Laparoendosc Adv Surg Tech A. 2000;10(2):71-3. doi: 10.1089/lap.2000.10.71.
Spitz JD, Arregui ME. Sutureless laparoscopic extraperitoneal inguinal herniorrhaphy using reusable instruments: two hundred three repairs without recurrence. Surg Laparosc Endosc Percutan Tech. 2000;10(1):24-9.
Tamme C, Scheidbach H, Hampe C, et al. Totally extraperitoneal endoscopic inguinal hernia repair (TEP). Surg Endosc. 2003;17(2):190-5. doi: 10.1007/s00464-002-8905-8.
Burcharth J. The epidemiology and risk factors for recurrence after inguinal hernia surgery. Dan Med J. 2014;61(5):B4846.
Petersen M, Friis-Andersen H, Zinther N. Does closure of the direct hernia defect in laparoscopic inguinal herniotomy reduce the risk of recurrence and seroma formation?: a systematic review and meta-analysis. Hernia. 2023;27(2):259-64. doi: 10.1007/s10029-022-02724-5.
Li J, Zhang W. Closure of a direct inguinal hernia defect in laparoscopic repair with barbed suture: a simple method to prevent seroma formation? Surg Endosc. 2018;32(2):1082-6. doi: 10.1007/s00464-017-5760-1.
Koyama T, Xiang Z, Nagai T, et al. Causes of peritoneal injury during laparoscopic totally extraperitoneal inguinal hernia repair and methods of repair. Asian J Endosc Surg. 2021;14(3):353-60. doi: 10.1111/ases.12869.
Donmez T, Karabulut M, Cayirci CE, et al. P-052 RISK FACTORS FOR PERITONEAL TEARS DURING LAPAROSCOPIC EXTRAPERITONEAL HERNIA REPAIR. Br J Surg. 2023.
Lau H, Patil NG, Yuen WK, et al. Management of peritoneal tear during endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc. 2002;16(10):1474-7. doi: 10.1007/s00464-001-8299-z.
Sawarkar P, Zade R, Dhamanaskar S, et al. Feasibility of laparoscopic inguinal hernia repair (TEP) in rural centre in India. Int Surg J. 2017;4(7):2336-41. doi: 10.18203/2349-2902.isj20172793.
Kochar S, Kakkar D, Singh DP. Evaluation of mesh fixation versus non-fixation in laparoscopic mesh hernioplasty in inguinal hernias. Int Surg J. 2020;7(10):3354-9. doi: 10.18203/2349-2902.isj20204136.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The Royal College of Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles must be contributed solely to The Thai Journal of Surgery and when published become the property of the Royal College of Surgeons of Thailand. The Royal College of Surgeons of Thailand reserves copyright on all published materials and such materials may not be reproduced in any form without the written permission.


