Pediatric Living Donor Liver Transplantation from Adult Allograft Liver After Resection of Focal Nodular Hyperplasia: The Report Three Cases
Keywords:
Living liver donor, Pediatric liver transplantation, Focal nodular hyperplasiaAbstract
Three pediatric living donor liver transplants were performed at Ramathibodi Hospital in Thailand. The recipients were two children with biliary atresia and one child with neonatal cholestasis jaundice with suspected biliary atresia. All three donors had a single liver lesion, which was suspected to be focal nodular hyperplasia (FNH) on preoperative imaging.
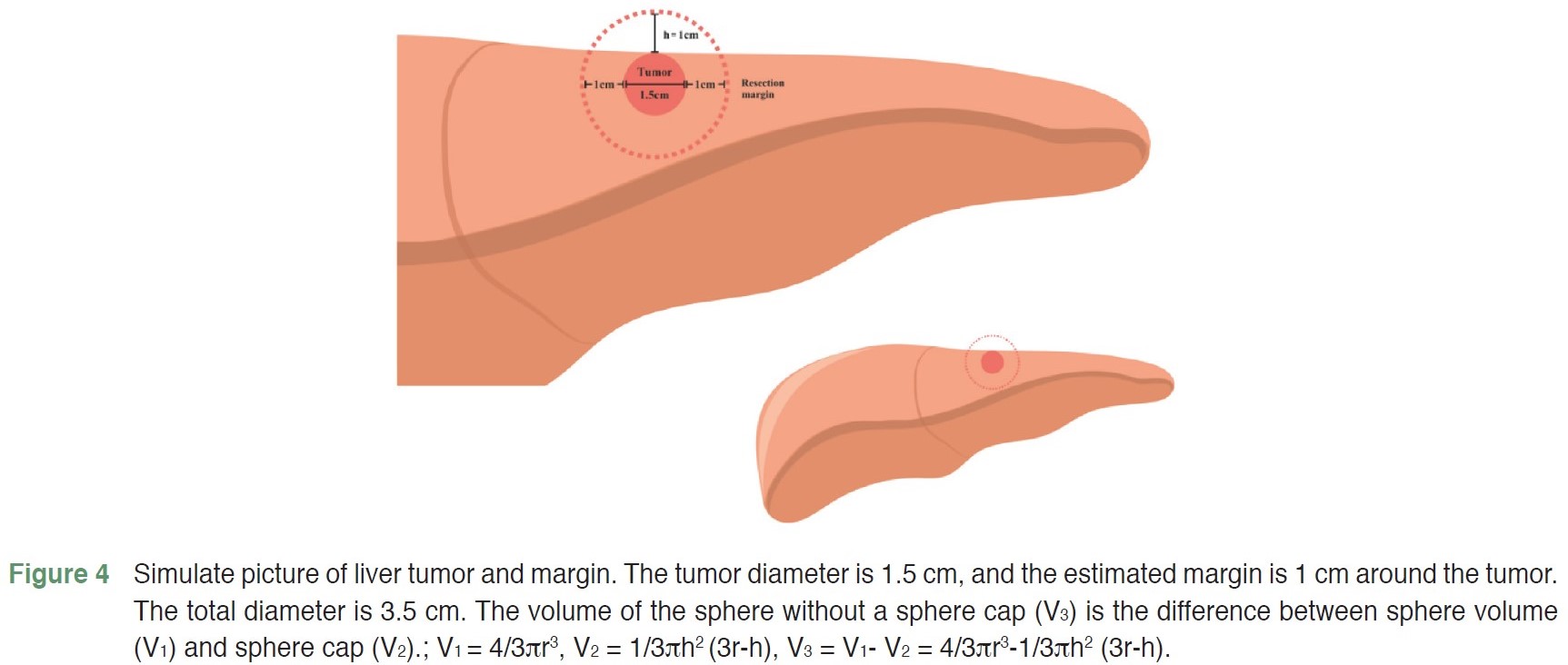
Because no other living donor candidates were available for the recipients, living donor liver transplants were performed. First, a wedge resection of the liver mass was performed. The liver mass was sent for a frozen section intraoperatively to confirm the diagnosis of a benign lesion and to ensure free-margin resection. Then, the transplantation was performed using a standard technique. The liver masses were 1.4-2.3 cm in diameter.
The liver donor hepatectomy was performed simultaneously with the recipient's total hepatectomy. The estimated liver graft volume was 176.5-336.5 cm3. The estimated graft-recipient weight ratio (GRWR) was 1.4-3.7%. The actual graft weight was 168-371 grams, and the actual GRWR was 1.6-3.5%. The liver graft was implanted in the recipient using a standard piggyback technique.
The donor and recipient were discharged after the operation without any complications. Follow-up ultrasound of the upper abdomen at six months showed no disease recurrence.
References
Rela M, Reddy MS. Living donor liver transplant (LDLT) is the way forward in Asia. Hepatol Int. 2017;11(2):148-51. doi: 10.1007/s12072-016-9780-z.
Chen CL, Kabiling CS, Concejero AM. Why does living donor liver transplantation flourish in Asia? Nat Rev Gastroenterol Hepatol. 2013;10(12):746-51. doi: 10.1038/nrgastro.2013.194.
Maillette de Buy Wenniger L, Terpstra V, Beuers U. Focal nodular hyperplasia and hepatic adenoma: epidemiology and pathology. Dig Surg. 2010;27(1):24-31. doi: 10.1159/000268404.
Tan M, Di Carlo A, Robinson P, et al. Successful outcome after transplantation of a donor liver with focal nodular hyperplasia. Liver Transpl. 2001;7(7):652-5. doi: 10.1053/jlts.2001.23910.
Gokcan H, Akdogan M, Kacar S, et al. Case of a successful liver transplantation from a living donor with focal nodular hyperplasia. Acta Gastroenterol Belg. 2016;79(2):262-3.
Li G, Mu X, Huang X, et al. Liver transplantation using the otherwise-discarded partial liver resection graft with hepatic benign tumor: Analysis of a preliminary experience on 15 consecutive cases. Medicine (Baltimore). 2017;96(29):e7295. doi: 10.1097/MD.0000000000007295.
Kasahara M, Sakamoto S. Optimal graft size in pediatric living donor liver transplantation: How are children different from adults? Pediatr Transplant. 2023;27(7):e14543. doi: 10.1111/petr.14543.
Goldaracena N, Echeverri J, Kehar M, et al. Pediatric living donor liver transplantation with large-for-size left lateral segment grafts. Am J Transplant. 2020;20(2):504-12. doi: 10.1111/ajt.15609.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The Royal College of Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles must be contributed solely to The Thai Journal of Surgery and when published become the property of the Royal College of Surgeons of Thailand. The Royal College of Surgeons of Thailand reserves copyright on all published materials and such materials may not be reproduced in any form without the written permission.


