Laparoscopic Surgery for Groin Hernia Repair: Single-Center Experience
Keywords:
Inguinal hernia, Laparoscopic, TAPP, TEP, ComplicationsAbstract
Background: Inguinal hernia arises from a condition characterized by a weakened abdominal wall. Laparoscopic inguinal hernia surgery is one treatment option. Due to the increasing use of laparoscopic inguinal hernia repair at Srinagarind Hospital, we are interested in studying these patients' side effects and treatment outcomes.
Materials and Methods: A descriptive study collected data between December 2011 and May 2022 at Srinagarind Hospital, Khon Kaen University. The medical records were reviewed, and data was collected. Descriptive statistics were used to analyze the data and report the side effects and treatment outcomes.
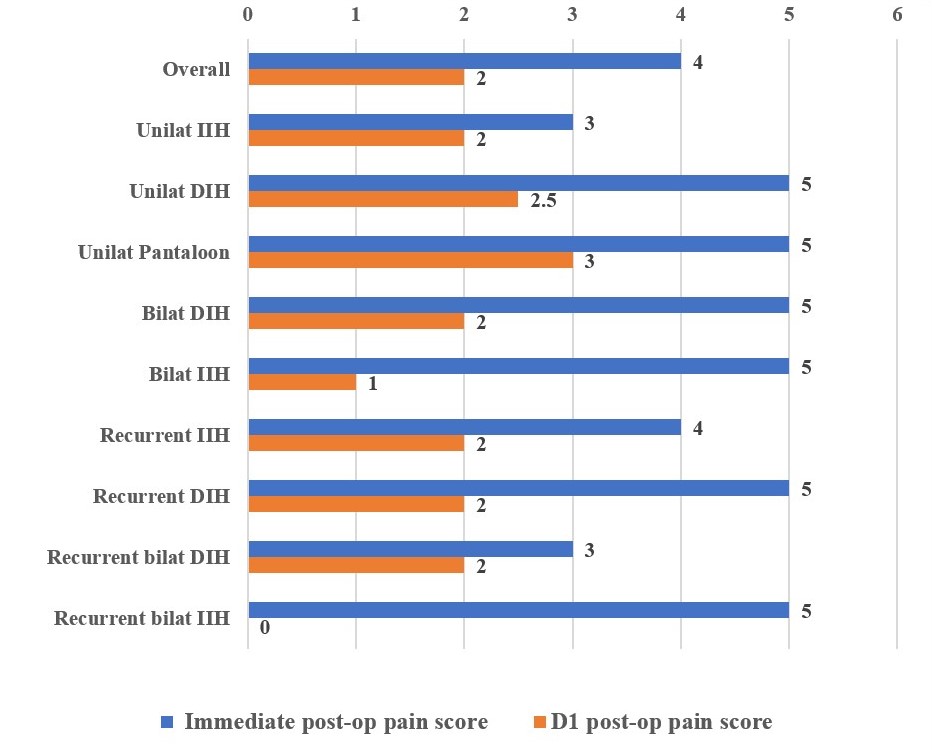
Results: A total of 269 patients underwent laparoscopic inguinal hernia repair. Among these patients, 251 were males (93.31%), and 18 were females (6.69%). The median age of the patients was 64 (IQR, 54-71). The most common comorbidities were hypertension (36.43%) and benign prostatic hyperplasia (BPH) (26.32%). The most common diagnosis was indirect inguinal hernia (40.89%). The overall median operative time was 65 minutes (IQR, 55-90). The median blood loss during the procedure was 5 milliliters (IQR, 5-10). The most common complication observed was hematoma, which occurred in approximately 16 cases (5.95%). Infection occurred in two cases (0.74%), and the recurrence rate was 1.49%.
Conclusions: Laparoscopic surgery for inguinal hernia repair was found to be efficient, safe, and comparable to other international studies regarding complications and recurrent rates, with no reported mortality.
References
HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22(1):1-165. doi: 10.1007/s10029-017-1668-x.
Zollinger RM Jr. An updated traditional classification of inguinal hernias. Hernia. 2004;8(4):318-22. doi: 10.1007/s10029-004-0245-2.
Haladu N, Alabi A, Brazzelli M, et al. Open versus laparoscopic repair of inguinal hernia: an overview of systematic reviews of randomised controlled trials. Surg Endosc. 2022;36(7):4685-4700. doi: 10.1007/s00464-022-09161-6.
McKernan JB, Laws HL. Laparoscopic repair of inguinal hernias using a totally extraperitoneal prosthetic approach. Surg Endosc. 1993;7(1):26-8. doi: 10.1007/BF00591232.
Ferzli G, Sayad P, Huie F, et al. Endoscopic extraperitoneal herniorrhaphy. A 5-year experience. Surg Endosc. 1998;12(11):1311-3. doi: 10.1007/s004649900847.
Wake BL, McCormack K, Fraser C, et al. Transabdominal pre-peritoneal (TAPP) vs totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2005;2005(1):CD004703. doi: 10.1002/14651858.CD004703.pub2.
Vader VL, Vogt DM, Zucker KA, et al. Adhesion formation in laparoscopic inguinal hernia repair. Surg Endosc. 1997;11(8):825-9. doi: 10.1007/s004649900463.
Rosenberg J, Bisgaard T, Kehlet H, et al. Danish Hernia Database recommendations for the management of inguinal and femoral hernia in adults. Dan Med Bull. 2011;58(2):C4243.
Simons MP, Aufenacker T, Bay-Nielsen M, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13(4):343-403. doi: 10.1007/s10029-009-0529-7.
Society for Surgery of the Alimentary Tract. SSAT patient care guidelines. Surgical repair of groin hernias. J Gastrointest Surg. 2007;11(9):1228-30. doi: 10.1007/s11605-007-0199-7.
Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet. 2003;362(9395):1561-71. doi: 10.1016/S0140-6736(03)14746-0.
Zhu X, Cao H, Ma Y, et al. Totally extraperitoneal laparoscopic hernioplasty versus open extraperitoneal approach for inguinal hernia repair: a meta-analysis of outcomes of our current knowledge. Surgeon. 2014;12(2):94-105. doi: 10.1016/j.surge.2013.11.018.
Voitk AJ. The learning curve in laparoscopic inguinal hernia repair for the community general surgeon. Can J Surg. 1998;41(6):446-50.
Solaini L, Cavaliere D, Avanzolini A, et al. Robotic versus laparoscopic inguinal hernia repair: an updated systematic review and meta-analysis. J Robot Surg. 2022;16(4):775-781. doi: 10.1007/s11701-021-01312-6.
Aghayeva A, Benlice C, Bilgin IA, et al. Laparoscopic totally extraperitoneal vs robotic transabdominal preperitoneal inguinal hernia repair: Assessment of short- and long-term outcomes. Int J Med Robot. 2020;16(4):e2111. doi: 10.1002/rcs.2111.
Holleran TJ, Napolitano MA, Sparks AD, et al. Trends and outcomes of open, laparoscopic, and robotic inguinal hernia repair in the veterans affairs system. Hernia. 2022;26(3):889-99. doi: 10.1007/s10029-021-02419-3.
Chen WL, Deng QQ, Xu W, et al. Multifactor study of efficacy and recurrence in laparoscopic surgery for inguinal hernia. World J Clin Cases. 2021;9(15):3559-66. doi: 10.12998/wjcc.v9.i15.3559.
Ates M, Kinaci E, Kose E, et al. Corona mortis: in vivo anatomical knowledge and the risk of injury in totally extraperitoneal inguinal hernia repair. Hernia. 2016;20(5):659-65. doi: 10.1007/s10029-015-1444-8.
Aiolfi A, Cavalli M, Ferraro SD, et al. Treatment of Inguinal Hernia: Systematic Review and Updated Network Meta-analysis of Randomized Controlled Trials. Ann Surg. 2021;274(6):954-61. doi: 10.1097/SLA.0000000000004735.
Wellwood J, Sculpher MJ, Stoker D, et al. Randomised controlled trial of laparoscopic versus open mesh repair for inguinal hernia: outcome and cost. BMJ. 1998;317(7151):103-10. doi: 10.1136/bmj.317.7151.103. Erratum in: BMJ 1998 Sep 5;317(7159):631.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The Royal College of Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles must be contributed solely to The Thai Journal of Surgery and when published become the property of the Royal College of Surgeons of Thailand. The Royal College of Surgeons of Thailand reserves copyright on all published materials and such materials may not be reproduced in any form without the written permission.


