Rare Axillary Cancer of Unknown Primary Originating from the Breast in Male Patient with PALB2 Pathogenic Variants: A Case Report
Cancer of Unknown Primary
Keywords:
Cancer of unknown primary, (PALB2) pathogenic variants, Male breast cancerAbstract
Abstract
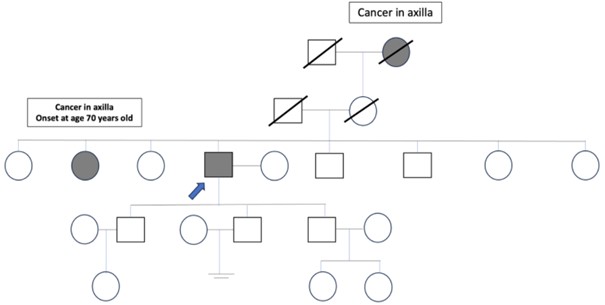
Background: Cancer of unknown primary (CUP) accounts for less than 5% of all cancers. Male breast cancer is a rare disease. The occurrence of bilateral breast involvement is even rarer, at approximately 0.5-2.5%. Genetic factors contribute to about 5-10%, with partner and localizer of BRCA2(PALB2) gene mutations accounting for 1-2%.
Case Report: We found a male with breast cancer who initially presented with metastatic adenocarcinoma at the axillary lymph node of unknown primary origin. After axillary lymph node dissection (ALND) with radiation therapy (RT), adjuvant chemotherapy, and regular surveillance, recurrence was observed on the same other side as the axillary lymph node. The PALB2 gene abnormality was also identified. Finally, he underwent prophylactic bilateral mastectomy, and the pathology report included bilateral benign breast tissue.
Conclusion: Patients without Breast cancer gene (BRCA)mutations should be offered next-generation sequencing (NGS) multi-gene panel testing to detect other abnormalities when personal is suggestive of a hereditary syndrome. The roles of bilateral prophylactic mastectomy, ALND, and RT will be discussed with the patient.
References
Krämer A, Bochtler T, Pauli C, et al. Electronic address: clinicalguidelines@esmo.org. Cancer of unknown primary: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. 2023;34(3):228-46. doi: 10.1016/j.annonc.2022.11.013.
Iyer P, Jasem J, Springer MA, et al. PALB2-Positive Breast Cancer in a 40-Year-Old Man. Oncology (Williston Park). 2017;31(1):50-2, 54.
Massard C, Loriot Y, Fizazi K. Carcinomas of an unknown primary origin--diagnosis and treatment. Nat Rev Clin Oncol. 2011;8(12):701-10. doi: 10.1038/nrclinonc.2011.158.
Fentiman IS, Fourquet A, Hortobagyi GN. Male breast cancer. Lancet. 2006;367(9510):595-604. doi: 10.1016/S0140-6736(06)68226-3. Erratum in: Lancet. 2006;367(9525):1818.
Evans DG, Susnerwala I, Dawson J, et al. Risk of breast cancer in male BRCA2 carriers. J Med Genet. 2010;47(10):710-1. doi: 10.1136/jmg.2009.075176.
Wolpert N, Warner E, Seminsky MF, et al. Prevalence of BRCA1 and BRCA2 mutations in male breast cancer patients in Canada. Clin Breast Cancer. 2000;1(1):57-63; discussion 64-5. doi: 10.3816/CBC.2000.n.005.
Kansuttiviwat C, Lertwilaiwittaya P, Roothumnong E, et al. Germline mutations of 4567 patients with hereditary breast-ovarian cancer spectrum in Thailand. NPJ Genom Med. 2024;9(1):9. doi: 10.1038/s41525-024-00400-4.
Szwiec M, Tomiczek-Szwiec J, Kluźniak W, et al. Genetic predisposition to male breast cancer in Poland. BMC Cancer. 2021;21(1):975. doi: 10.1186/s12885-021-08718-3.
Vietri MT, Caliendo G, D'Elia G, et al. BRCA and PALB2 mutations in a cohort of male breast cancer with one bilateral case. Eur J Med Genet. 2020;63(6):103883. doi: 10.1016/j.ejmg.2020.103883.
Ding YC, Steele L, Kuan CJ, et al. Mutations in BRCA2 and PALB2 in male breast cancer cases from the United States. Breast Cancer Res Treat. 2011;126(3):771-8. doi: 10.1007/s10549-010-1195-2.
De Angelis C, Nardelli C, Concolino P, et al. Case Report: Detection of a Novel Germline PALB2 Deletion in a Young Woman With Hereditary Breast Cancer: When the Patient's Phenotype History Doesn't Lie. Front Oncol. 2021;11:602523. doi: 10.3389/fonc.2021.602523.
Cortesi L, Piombino C, Toss A. Germline Mutations in Other Homologous Recombination Repair-Related Genes Than BRCA1/2: Predictive or Prognostic Factors? J Pers Med. 2021;11(4):245. doi: 10.3390/jpm11040245.
Sun Y, McCorvie TJ, Yates LA, et al. Structural basis of homologous recombination. Cell Mol Life Sci. 2020;77(1):3-18. doi: 10.1007/s00018-019-03365-1.
Toss A, Ponzoni O, Riccò B, et al. Management of PALB2-associated breast cancer: A literature review and case report. Clin Case Rep. 2023;11(8):e7747. doi: 10.1002/ccr3.7747.
Macedo FI, Eid JJ, Flynn J, et al. Optimal Surgical Management for Occult Breast Carcinoma: A Meta-analysis. Ann Surg Oncol. 2016;23(6):1838-44. doi: 10.1245/s10434-016-5104-8.
Kim H, Park W, Kim SS, et al. Prognosis of patients with axillary lymph node metastases from occult breast cancer: analysis of multicenter data. Radiat Oncol J. 2021;39(2):107-12. doi: 10.3857/roj.2021.00241.
Yang X, Leslie G, Doroszuk A, et al. Cancer Risks Associated With Germline PALB2 Pathogenic Variants: An International Study of 524 Families. J Clin Oncol. 2020;38(7):674-85. doi: 10.1200/JCO.19.01907.
National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) in Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic (Version 1.2025); 2024. [cited 2024 September 11]. Available from: https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1503.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The Royal College of Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles must be contributed solely to The Thai Journal of Surgery and when published become the property of the Royal College of Surgeons of Thailand. The Royal College of Surgeons of Thailand reserves copyright on all published materials and such materials may not be reproduced in any form without the written permission.


