The Success Rate and Complications of Central Venous Catheterization for General Surgery Patients in a Tertiary Hospital
Keywords:
Success rate, Complications, Central venous catheterization (CVC)Abstract
Objective: Central venous catheterization (CVC) is one of the essential surgical procedures. It can lead to life-threatening complications. This prospective study aimed to evaluate the success rate and complications of central venous catheterization.
Methods: This prospective observational cohort study collected data from patients undergoing central venous catheterization at the General Surgery Department, Rajavithi Hospital, from October 2020 to September 2022. Demographic information, the number of insertion attempts, operator details, success rates, the method used (ultrasound (US)-guided or anatomical landmark), and complications were recorded. Data analysis employed descriptive statistics, chi-square tests, student’s t-tests, and binary logistic regression.
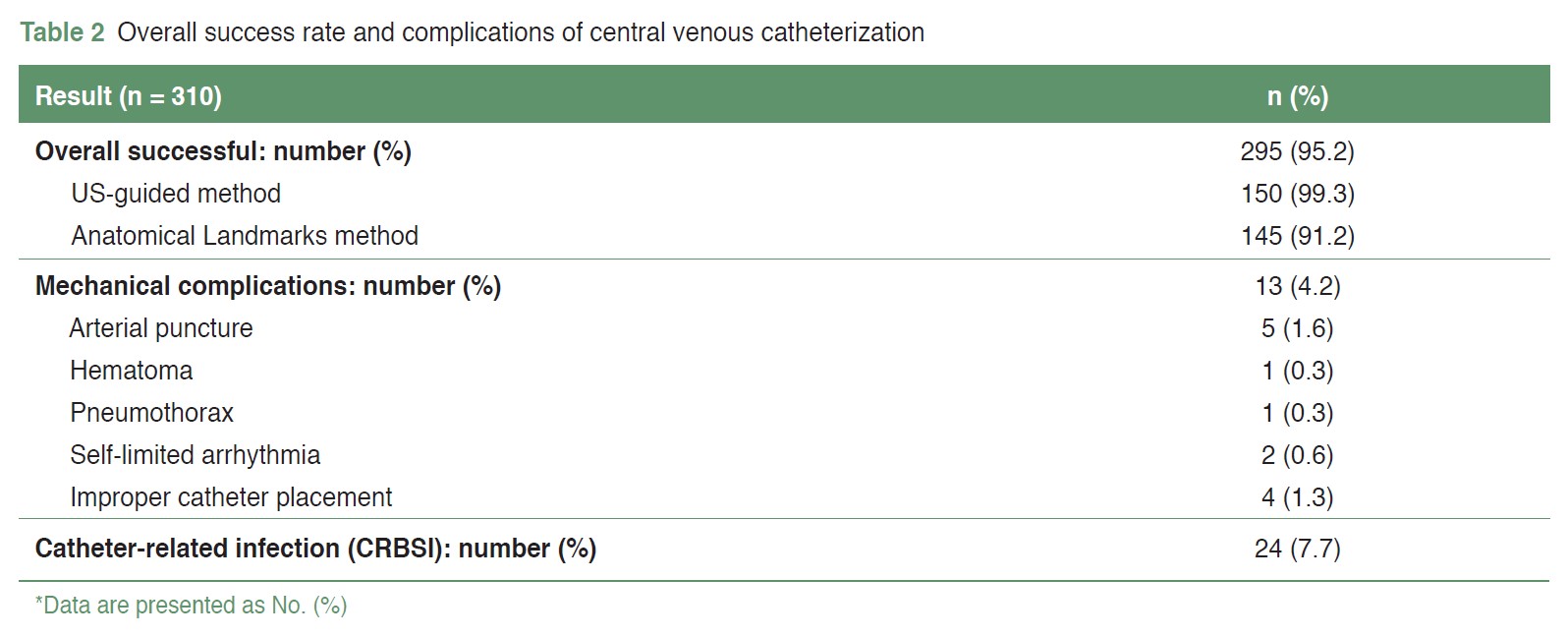
Result: 310 patients were enrolled. The overall success rate for central venous catheter (CVC) insertion was 95.2%. The US-guided method showed a significantly higher success rate compared to the anatomical landmark method (99.3% vs. 91.2%, P = 0.001), with 82.1% catheterized successfully on the first attempt using the US-guidance versus 50.9% with the landmark method (P < 0.001). The overall mechanical complication rate was 4.2%, including arterial puncture (1.6%), hematoma (0.3%), pneumothorax (0.3%), self-limiting arrhythmias (0.6%), and improper catheter placement (1.3%). The CRBSI rate was 7.7%, higher when occurring more than 15 days post-insertion (P < 0.001). Complication rates were significantly lower with the US-guided method compared to the landmark method (0.7% vs. 7.5%, P = 0.003). Procedures performed by 3rd to 4th-year residents also had lower complication rates compared to 1st to 2nd-year residents (0.3% vs. 3.9%, P = 0.023).
Conclusion: The US-guided catheterization demonstrates a high success rate, fewer attempts, and reduced complication rates. Therefore, its regular use in catheterization procedures is strongly recommended.
References
Wu SY, Ling Q, Cao LH, et al. Real-time two-dimensional ultrasound guidance for central venous cannulation: a meta-analysis. Anesthesiology. 2013;118(2):361-75. doi: 10.1097/ALN.0b013e31827bd172.
Ouriel K. Preventing complications of central venous catheterization. N Engl J Med. 2003;348(26):2684-6.
Parienti JJ, Mongardon N, Mégarbane B, et al. Intravascular Complications of Central Venous Catheterization by Insertion Site. N Engl J Med. 2015;373(13):1220-9. doi: 10.1056/NEJMoa1500964.
Bouaziz H, Zetlaoui PJ, Pierre S, et al. Guidelines on the use of ultrasound guidance for vascular access. Anaesth Crit Care Pain Med. 2015;34(1):65-9. doi: 10.1016/j.accpm.2015.01.004.
Timsit JF, Baleine J, Bernard L, et al. Expert consensus-based clinical practice guidelines management of intravascular catheters in the intensive care unit. Ann Intensive Care. 2020;10(1):118. doi: 10.1186/s13613-020-00713-4.
Lamperti M, Biasucci DG, Disma N, et al. European Society of Anaesthesiology guidelines on peri-operative use of ultrasound-guided for vascular access (PERSEUS vascular access). Eur J Anaesthesiol. 2020;37(5):344-76. doi: 10.1097/EJA.0000000000001180.
Practice Guidelines for Central Venous Access 2020: An Updated Report by the American Society of Anesthesiologists Task Force on Central Venous Access. Anesthesiology. 2020;132(1):8-43. doi: 10.1097/ALN.0000000000002864.
The Seldinger technique. Reprint from Acta Radiologica 1953. AJR Am J Roentgenol. 1984;142(1):5-7. doi: 10.2214/ajr.142.1.5.
Shiloh AL, Savel RH, Paulin LM, et al. Ultrasound-guided catheterization of the radial artery: a systematic review and meta-analysis of randomized controlled trials. Chest. 2011;139(3):524-9. doi: 10.1378/chest.10-0919.
Eisen LA, Narasimhan M, Berger JS, et al. Mechanical complications of central venous catheters. J Intensive Care Med. 2006;21(1):40-6. doi: 10.1177/0885066605280884.
Airapetian N, Maizel J, Langelle F, et al. Ultrasound-guided central venous cannulation is superior to quick-look ultrasound and landmark methods among inexperienced operators: a prospective randomized study. Intensive Care Med. 2013;39(11):1938-44. doi: 10.1007/s00134-013-3072-z.
Verghese ST, McGill WA, Patel RI, et al. Ultrasound-guided internal jugular venous cannulation in infants: a prospective comparison with the traditional palpation method. Anesthesiology. 1999;91(1):71-7. doi: 10.1097/00000542-199907000-00013.
Mitre CI, Golea A, Acalovschi I, et al. Ultrasound-guided external jugular vein cannulation for central venous access by inexperienced trainees. Eur J Anaesthesiol. 2010;27(3):300-3. doi: 10.1097/EJA.0b013e328333c2d6.
Mey U, Glasmacher A, Hahn C, et al. Evaluation of an ultrasound-guided technique for central venous access via the internal jugular vein in 493 patients. Support Care Cancer. 2003;11(3):148-55. doi: 10.1007/s00520-002-0399-3.
Theodoro D, Krauss M, Kollef M, et al. Risk factors for acute adverse events during ultrasound-guided central venous cannulation in the emergency department. Acad Emerg Med. 2010;17(10):1055-61. doi: 10.1111/j.1553-2712.2010.00886.x.
Mansfield PF, Hohn DC, Fornage BD, et al. Complications and failures of subclavian-vein catheterization. N Engl J Med. 1994;331(26):1735-8. doi: 10.1056/NEJM199412293312602.
Hind D, Calvert N, McWilliams R, et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ. 2003;327(7411):361. doi: 10.1136/bmj.327.7411.361.
Miller AH, Roth BA, Mills TJ, et al. Ultrasound guidance versus the landmark technique for the placement of central venous catheters in the emergency department. Acad Emerg Med. 2002;9(8):800-5. doi: 10.1111/j.1553-2712.2002.tb02168.x.
Karakitsos D, Labropoulos N, De Groot E, et al. Real-time ultrasound-guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006;10(6):R162. doi: 10.1186/cc5101.
Rando K, Castelli J, Pratt JP, et al. Ultrasound-guided internal jugular vein catheterization: a randomized controlled trial. Heart Lung Vessel. 2014;6(1):13-23.
Randolph AG, Cook DJ, Gonzales CA, et al. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med. 1996;24(12):2053-8. doi: 10.1097/00003246-199612000-00020.
Calvert N, Hind D, McWilliams RG, et al. The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation. Health Technol Assess. 2003;7(12):1-84. doi: 10.3310/hta7120.
Feller-Kopman D. Ultrasound-guided internal jugular access: a proposed standardized approach and implications for training and practice. Chest. 2007;132(1):302-9. doi: 10.1378/chest.06-2711.
Madenci AL, Solis CV, de Moya MA. Central venous access by trainees: a systematic review and meta-analysis of the use of simulation to improve success rate on patients. Simul Healthc. 2014;9(1):7-14. doi: 10.1097/SIH.0b013e3182a3df26.
Maizel J, Guyomarc'h L, Henon P, et al. Residents learning ultrasound-guided catheterization are not sufficiently skilled to use landmarks. Crit Care. 2014;18(1):R36. doi: 10.1186/cc13741.
Takeshita J, Tachibana K, Nakajima Y, et al. Incidence of catheter-related bloodstream infections following ultrasound-guided central venous catheterization: a systematic review and meta-analysis. BMC Infect Dis. 2022;22(1):772. doi: 10.1186/s12879-022-07760-1.
Buetti N, Mimoz O, Mermel L, et al. Ultrasound Guidance and Risk for Central Venous Catheter-Related Infections in the Intensive Care Unit: A Post Hoc Analysis of Individual Data of 3 Multicenter Randomized Trials. Clin Infect Dis. 2021;73(5):e1054-e1061. doi: 10.1093/cid/ciaa1817.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The Royal College of Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles must be contributed solely to The Thai Journal of Surgery and when published become the property of the Royal College of Surgeons of Thailand. The Royal College of Surgeons of Thailand reserves copyright on all published materials and such materials may not be reproduced in any form without the written permission.


