Effects of nasal continuous positive airway pressure compared with high flow nasal cannula on the coordination between swallowing and breathing in post-extubation patients, a randomized crossover study
Swallowing–breathing coordination with CPAP vs HFNC
DOI:
https://doi.org/10.54205/ccc.v33.275059Keywords:
Continuous positive airway pressure, High flow nasal cannula, Coordination of breathing and swallowing, Post-extubationAbstract
Background: Coordination between swallowing and breathing is essential to prevent aspiration. Swallowing during expiration (E-E swallow) is considered the most protective pattern [1,2]. High-flow nasal cannula (HFNC) and continuous positive airway pressure (CPAP) may promote this pattern by increasing the proportion of E-E swallows [3-5], but their comparative effects in post-extubation patients remain unclear.
Objectives: To compare the effects of nasal CPAP and HFNC on swallowing-breathing coordination patterns in post-extubation patients and to identify factors influencing this coordination
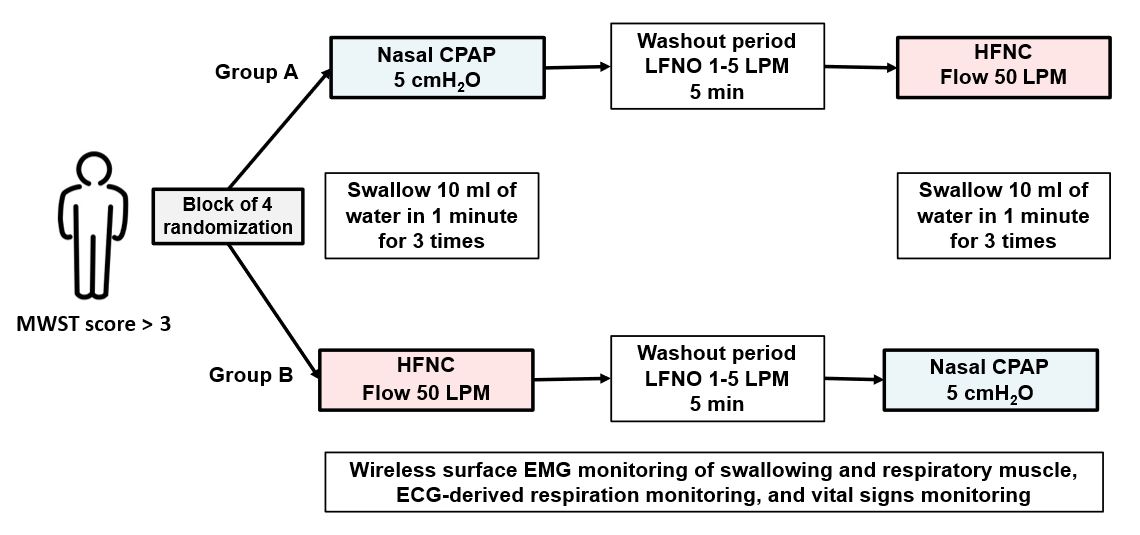
Methods: This randomized, controlled, crossover trial includes patients who received invasive mechanical ventilation for ≥ 48 hours and were extubated within 48 hours prior to enrollment. Patients with dysphagia (modified water swallowing test score < 4) were excluded. Eligible patients are randomly assigned to Group A (CPAP → HFNC) or Group B (HFNC → CPAP). Each intervention is applied for 5 minutes, followed by three continuous water swallowing tests. Swallowing and respiratory phases are recorded using surface EMG and ECG-derived respiration. A 5-minute washout with low-flow nasal oxygen is provided between interventions. Swallowing–breathing coordination is classified into four patterns: E–E, I–E, E–I, and I–I. The primary outcome is the percentage of E-E swallows. Secondary outcomes include other patterns, swallowing frequency, expiratory time, and respiratory rate. All outcomes are analyzed using linear mixed-effects models.
Hypothesis: CPAP and HFNC may differ in their effects on swallowing–breathing coordination, particularly in promoting the E–E pattern.
Conclusion: This study explores how nasal CPAP and HFNC affect swallowing–breathing coordination and their potential impact on airway protection after extubation.
Ethics and dissemination: Approved by the IRB, Faculty of Medicine, Chulalongkorn University. Results will be disseminated via peer-reviewed journals and conferences.
Trial registration: TCTR20210607003
Downloads
References
Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008;19:691-707.
Matsuo K, Palmer JB. Coordination of Mastication, Swallowing and Breathing. Jpn Dent Sci Rev. 2009;45:31-40.
Hori R, Isaka M, Oonishi K, Yabe T, Oku Y. Coordination between respiration and swallowing during non-invasive positive pressure ventilation. Respirology. 2016;21:1062-7.
Hori R, Ishida R, Isaka M, Nakamura T, Oku Y. Effects of noninvasive ventilation on the coordination between breathing and swallowing in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2019;14:1485-94.
Rattanajiajaroen P, Kongpolprom N. Effects of high flow nasal cannula on the coordination between swallowing and breathing in postextubation patients, a randomized crossover study. Crit Care. 2021;25:365.
Fernando SM, Seely AJE. Post-extubation dysphagia: the truth is hard to swallow. Chest. 2020;158:1806-7.
Brodsky MB, Nollet JL, Spronk PE, Gonzalez-Fernandez M. Prevalence, pathophysiology, diagnostic modalities, and treatment options for dysphagia in critically ill patients. Am J Phys Med Rehabil. 2020;99:1164-70.
Sanuki T, Mishima G, Kiriishi K, Watanabe T, Okayasu I, Kawai M, et al. Effect of nasal high-flow oxygen therapy on the swallowing reflex: an in vivo volunteer study. Clin Oral Investig. 2017;21:915-20.
Ferrer M, Valencia M, Nicolas JM, Bernadich O, Badia JR, Torres A. Early noninvasive ventilation averts extubation failure in patients at risk: a randomized trial. Am J Respir Crit Care Med. 2006;173:164-70.
Hernandez G, Vaquero C, Gonzalez P, Subira C, Frutos-Vivar F, Rialp G, et al. Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA. 2016;315:1354-61.
Hernandez G, Vaquero C, Colinas L, Cuena R, Gonzalez P, Canabal A, et al. Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients: a randomized clinical trial. JAMA. 2016;316:1565-74.
Nava S, Gregoretti C, Fanfulla F, Squadrone E, Grassi M, Carlucci A, et al. Noninvasive ventilation to prevent respiratory failure after extubation in high-risk patients. Crit Care Med. 2005;33:2465-70.
Wellek S, Blettner M. On the proper use of the crossover design in clinical trials: part 18 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2012;109:276-81.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 The Thai Society of Critical Care Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.




