Irritant and asphyxiant gases
Irritant and asphyxiant gases
DOI:
https://doi.org/10.54205/ccc.v33.273625คำสำคัญ:
Asphyxiants, Carbon monoxide, Cyanide, Hydrogen sulfide, Methemoglobinemia, Respiratory irritantsบทคัดย่อ
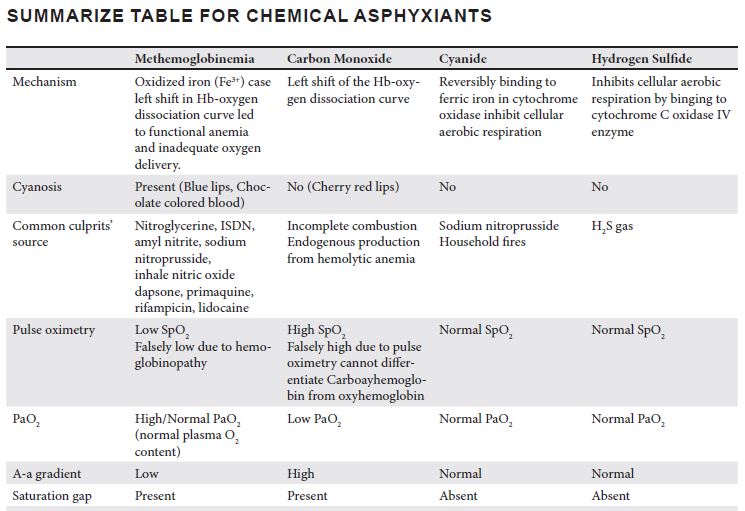
Both irritant and asphyxiant gases are hazardous substances that, when inhaled, can cause a spectrum of respiratory complications, ranging from mild irritation to life-threatening respiratory failure. These gases are classified into three main categories based on their mechanisms of toxicity: pulmonary irritants, simple asphyxiants, and chemical asphyxiants. Pulmonary irritants, such as chlorine, phosgene, and ammonia, cause direct injury to the respiratory mucosa, leading to inflammation, bronchospasm, and pulmonary edema. Simple asphyxiants, including nitrogen, methane, and carbon dioxide, displace oxygen in the environment, resulting in hypoxia and potentially fatal respiratory depression. Chemical asphyxiants, such as carbon monoxide, hydrogen cyanide, and hydrogen sulfide, interfere with oxygen transport or cellular respiration, causing systemic hypoxia at the mitochondrial level.
Diagnosis of the gas exposure relies on a detailed history of exposure, clinical symptoms, and laboratory investigations, including arterial blood gas analysis, pulse oximetry, and carboxyhemoglobin or methemoglobin levels. Management involves immediate removal from the toxic environment, decontamination, oxygen supplementation, and supportive treatment. Specific antidotes, such as hydroxocobalamin for cyanide poisoning and methylene blue for methemoglobinemia, may be required in severe cases. Given the potential for rapid deterioration, early recognition and prompt intervention are essential in preventing morbidity and mortality. This review provides an in-depth analysis of the toxicology, pathophysiology, and management strategies associated with asphyxiant gas exposure.
Downloads
เอกสารอ้างอิง
do Pico GA. Toxic gas inhalation. Curr Opin Pulm Med. 1995;1:102-8.
Juneja D, Singh O. Principles and Practice of Critical Care Toxicology; 2019.
Charlton NP, Kirk MA. Smoke Inhalation. In: Nelson LS, Howland MA, Lewin NA, Smith SW, Goldfrank LR, Hoffman RS, editors. Goldfrank's Toxicologic Emergencies, 11e. New York, NY: McGraw-Hill Education; 2019.
Walker V. Ammonia metabolism and hyperammonemic disorders. Adv Clin Chem. 2014;67:73-150.
Weiner ID, Verlander JW. Renal ammonia metabolism and transport. Compr Physiol. 2013;3:201-20.
Helmers S, Top FH, Sr., Knapp LW, Jr. Ammonia injuries in agriculture. J Iowa Med Soc. 1971;61:271-80.
Dasarathy S, Mookerjee RP, Rackayova V, Rangroo Thrane V, Vairappan B, Ott P, et al. Ammonia toxicity: from head to toe? Metab Brain Dis. 2017;32:529-38.
de la Hoz RE, Schlueter DP, Rom WN. Chronic lung disease secondary to ammonia inhalation injury: a report on three cases. Am J Ind Med. 1996;29:209-14.
Padappayil RP, Borger J. Ammonia Toxicity. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2025, StatPearls Publishing LLC; 2025.
Registry AfTSaD. Medical Management Guidelines for Ammonia. [accessed Janurary 1, 2025, 2025]. Available at: https://wwwn.cdc.gov/TSP/MMG/MMGDetails.aspx?mmgid=7&toxid=2.
White CW, Martin JG. Chlorine gas inhalation: human clinical evidence of toxicity and experience in animal models. Proc Am Thorac Soc. 2010;7:257-63.
Morim A, Guldner GT. Chlorine Gas Toxicity. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2025, StatPearls Publishing LLC.; 2025.
Winder C. The Toxicology of Chlorine. Environmental Research. 2001;85:105-14.
Achanta S, Jordt SE. Toxic effects of chlorine gas and potential treatments: a literature review. Toxicol Mech Methods. 2021;31:244-56.
Das R, Blanc PD. Chlorine gas exposure and the lung: a review. Toxicol Ind Health 1993;9:439-55.
Bosse GM. Nebulized sodium bicarbonate in the treatment of chlorine gas inhalation. J Toxicol Clin Toxicol. 1994;32:233-41.
Aslan S, Kandiş H, Akgun M, Cakir Z, Inandi T, Görgüner M. The effect of nebulized NaHCO3 treatment on "RADS" due to chlorine gas inhalation. Inhal Toxicol. 2006;18:895-900.
Wang J, Winskog C, Edston E, Walther SM. Inhaled and intravenous corticosteroids both attenuate chlorine gas-induced lung injury in pigs. Acta Anaesthesiol Scand. 2005;49:183-90.
Long N. Chlorine toxicity. [accessed January 1, 2025. Available at: https://litfl.com/chlorine-toxicity/.
Vaish AK, Consul S, Agrawal A, Chaudhary SC, Gutch M, Jain N, et al. Accidental phosgene gas exposure: A review with background study of 10 cases. J Emerg Trauma Shock. 2013;6:271-5.
Von Zimmerman MA, Arnold TC. Phosgene Toxicity. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2025, StatPearls Publishing LLC.; 2025.
Registry AfTSaD. Medical Management Guidelines for Phosgene. Available at: https://wwwn.cdc.gov/TSP/MMG/MMGDetails.aspx?mmgid=1201&toxid=182
Cao C, Zhang L, Shen J. Phosgene-Induced acute lung injury: Approaches for mechanism-based treatment strategies. Front Immunol. 2022;13:917395.
Lu Q, Huang S, Meng X, Zhang J, Yu S, Li J, et al. Mechanism of Phosgene-Induced Acute Lung Injury and Treatment Strategy. Int J Mol Sci. 2021;22.
Spelce D, McKay RT, Johnson JS, Rehak TR, Metzler RW. Respiratory Protection for Oxygen Deficient Atmospheres. J Int Soc Respir Prot. 2016;33.
Varon J, Marik PE, Fromm RE, Jr., Gueler A. Carbon monoxide poisoning: a review for clinicians. J Emerg Med. 1999;17:87-93.
Temple AW. Methylene chloride. [accessed January 1, 2025. Available at: https://www.inchem.org/documents/pims/chemical/pim343.htm.
Hariri G, Hodjat Panah K, Beneteau-Burnat B, Chaquin M, Mekinian A, Ait-Oufella H. Carboxyhemoglobin, a reliable diagnosis biomarker for hemolysis in intensive care unit: a retrospective study. Crit Care. 2021;25:7.
Wang T, Zhang Y. Mechanisms and therapeutic targets of carbon monoxide poisoning: A focus on reactive oxygen species. Chemico-Biological Interactions. 2024;403:111223.
Guzman JA. Carbon Monoxide Poisoning. Critical Care Clinics. 2012;28:537-48.
Weaver LK. Clinical practice. Carbon monoxide poisoning. N Engl J Med. 2009;360:1217-25.
Rose JJ, Wang L, Xu Q, McTiernan CF, Shiva S, Tejero J, et al. Carbon Monoxide Poisoning: Pathogenesis, Management, and Future Directions of Therapy. Am J Respir Crit Care Med. 2017;195:596-606.
Hampson NB, Piantadosi CA, Thom SR, Weaver LK. Practice recommendations in the diagnosis, management, and prevention of carbon monoxide poisoning. Am J Respir Crit Care Med. 2012;186:1095-101.
Pace N, Strajman E, Walker EL. Acceleration of carbon monoxide elimination in man by high pressure oxygen. Science. 1950;111:652-4.
David S, Sawal NS, Hamzah MNSB, Rajabalaya R. The blood blues: A review on methemoglobinemia. J Pharmacol Pharmacother. 2018;9:1-5.
Sugavanam K. A comprehensive review on methemoglobinemia. 2021:108-12.
Iolascon A, Bianchi P, Andolfo I, Russo R, Barcellini W, Fermo E, et al. Recommendations for diagnosis and treatment of methemoglobinemia. Am J Hematol. 2021;96:1666-78.
Cefalu JN, Joshi TV, Spalitta MJ, Kadi CJ, Diaz JH, Eskander JP, et al. Methemoglobinemia in the Operating Room and Intensive Care Unit: Early Recognition, Pathophysiology, and Management. Adv Ther. 2020;37:1714-23.
Skold A, Cosco DL, Klein R. Methemoglobinemia: pathogenesis, diagnosis, and management. South Med J. 2011;104:757-61.
Lavonas EJ, Akpunonu PD, Arens AM, Babu KM, Cao D, Hoffman RS, et al. 2023 American Heart Association Focused Update on the Management of Patients With Cardiac Arrest or Life-Threatening Toxicity Due to Poisoning: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2023;148:e149-e84.
Jaszczak E, Polkowska Ż, Narkowicz S, Namieśnik J. Cyanides in the environment-analysis-problems and challenges. Environ Sci Pollut Res Int. 2017;24:15929-48.
Council NR. Acute Exposure Guideline Levels for Selected Airborne Chemicals: Volume 2. Washington, DC: The National Academies Press; 2002.
Hendry-Hofer TB, Ng PC, Witeof AE, Mahon SB, Brenner M, Boss GR, et al. A Review on Ingested Cyanide: Risks, Clinical Presentation, Diagnostics, and Treatment Challenges. J Med Toxicol. 2019;15:128-33.
Baud FJ, Borron SW, Mégarbane B, Trout H, Lapostolle F, Vicaut E, et al. Value of lactic acidosis in the assessment of the severity of acute cyanide poisoning. Crit Care Med. 2002;30:2044-50.
Reade MC, Davies SR, Morley PT, Dennett J, Jacobs IC. Review article: management of cyanide poisoning. Emerg Med Australas. 2012;24:225-38.
Beasley DM, Glass WI. Cyanide poisoning: pathophysiology and treatment recommendations. Occup Med (Lond). 1998;48:427-31.
Registry AfTSaD. Medical Management Guidelines for Hydrogen Cyanide. [accessed January 1, 2025. Available at: https://wwwn.cdc.gov/TSP/MMG/MMGDetails.aspx?mmgid=1141&toxid=249.
Holstege CP, Kirk MA. Cyanide and Hydrogen Sulfide. In: Nelson LS, Howland MA, Lewin NA, Smith SW, Goldfrank LR, Hoffman RS, editors. Goldfrank's Toxicologic Emergencies, 11e. New York, NY: McGraw-Hill Education; 2019.
Anseeuw K, Delvau N, Burillo-Putze G, De Iaco F, Geldner G, Holmström P, et al. Cyanide poisoning by fire smoke inhalation: a European expert consensus. Eur J Emerg Med. 2013;20:2-9.
Rumbeiha W, Whitley E, Anantharam P, Kim DS, Kanthasamy A. Acute hydrogen sulfide-induced neuropathology and neurological sequelae: challenges for translational neuroprotective research. Ann N Y Acad Sci. 2016;1378:5-16.
Guidotti TL. Hydrogen sulfide: advances in understanding human toxicity. Int J Toxicol. 2010;29:569-81.
Jiang J, Chan A, Ali S, Saha A, Haushalter KJ, Lam WL, et al. Hydrogen Sulfide--Mechanisms of Toxicity and Development of an Antidote. Sci Rep. 2016;6:20831.
Skolnik A, Heise CW. Hydrogen Sulfide. In: Brent J, Burkhart K, Dargan P, Hatten B, Megarbane B, Palmer R, White J, editors. Critical Care Toxicology: Diagnosis and Management of the Critically Poisoned Patient. Cham: Springer International Publishing; 2017. p 1963-71.
Registry AfTSaD. Medical Management Guidelines for Hydrogen Sulfide. Available at: https://wwwn.cdc.gov/TSP/MMG/MMGDetails.aspx?mmgid=385&toxid=67
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
ลิขสิทธิ์ (c) 2025 สมาคมเวชบำบัดวิกฤตแห่งประเทศไทย

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial 4.0 International License.




