EFFECT OF THAI BOXING EXERCISE TRAINING ON MAXIMAL VENTILATION IN OBESE SUBJECTS
Main Article Content
Abstract
Purpose The purpose of this study was to investigate the effects of Thai boxing exercise training on the maximal minute ventilation in the first degree obese participants.
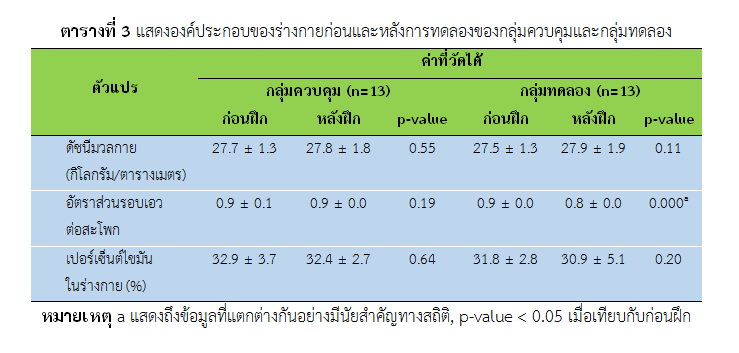
Methods Twenty-six of the first degree obesity participants (males=6 and females=20) was selected by simple random sampling using computer and was divided into 2 groups, the control group (CG; n=13) (age = 20.7±1.4 yrs and BMI = 27.6±1.2 kg.m-2) and the boxing training group (TG; n=13) (age = 20.2±1.1 yrs and BMI = 27.5±1.3 kg.m-2). The maximal minute ventilation was assessed using ramp incremental cycling test before (pre) and after the 8 weeks of training (post). The CG had performed a normal daily life in 8 weeks. The TG was trained by using Thai boxing exercising at 89±4 percent of maximum heart rate. Boxing time was 3 minutes and switch time 4 minutes per round that amount 2-5 rounds per time with had duration 54-75 minutes per day, 3 days per week that had totally 8 weeks. The data was analyzed by mixed model ANOVA which had statistical significance at p-value < 0.05. This study had been approved by the Naresuan University Research Ethics Committee (IRB No.242/2017; October 11, 2017).
Results The results revealed that pre-test parameters were not different between the two groups. After the 8 weeks of training, the TG had significant higher in the maximal minute ventilation than the CG (TG = 82.0±23.2 L.min-2 vs CG = 60.1±19.3 L.min-2) (p-value<0.05). Moreover, the TG demonstrated significantly improve in the maximal minute ventilation after training when compared to before training (pre-test = 59.3±14.5 L.min-2 vs post-test = 81.9±23.1 L.min-2) (p-value < 0.05) whereas no improved were detected for CG when compared to before training (p-value>0.05)
Article Details
References
American College of Sports Medicine. (1998). American College of Sports Medicine Position Stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc, 30(6), 975-991.
American College of Sports Medicine. (2010). ACSM’s guidelines for exercise testing and prescription (8 ed.). Philadelphia: Lippincott Williams & Wilkins.
Arseneau, E., Mekary, S., & Leger, L. A. (2011). VO(2) requirements of boxing exercises. J Strength Cond Res, 25(2), 348-359.
Boutcher, S. H. (2011). High-intensity intermittent exercise and fat loss. J Obes, 2011, 1-10.
Chaiut., W., Paungmali., A., & Sitilertpisan., P. (2014). Effects of aerobic exercise with core muscle training on cardiopulmonary system in healthy individuals. Journal of Sports Science and Technology, 14(2), 91-103.
Chaiwanichsiri, D. (2010). Rehabilitation medicine. Bangkok: Department of Rehabilitation Medicine Faculty of Medicine Chulalongkorn University.
Cheema, B. S., Davies, T. B., Stewart, M., Papalia, S., & Atlantis, E. (2015). The feasibility and effectiveness of high-intensity boxing training versus moderate-intensity brisk walking in adults with abdominal obesity: a pilot study. BMC Sports Sci Med Rehabil, 7(3), 1-8.
Crisafulli, A., Vitelli, S., Cappai, I., Milia, R., Tocco, F., Melis, F., & Concu, A. (2009). Physiological responses and energy cost during a simulation of a Muay Thai boxing match. Appl Physiol Nutr Metab, 34(2), 143-150.
Ghouse, M. S., Surekha.B.Barwal, & Amruta.S.Wattamwar. (2016). A Review on Obesity. Health Science Journal, 10(4.13), 1-5.
Hebisz, P., Hebisz, R., Zaton, M., Ochmann, B., & Mielnik, N. (2016). Concomitant application of sprint and high-intensity interval training on maximal oxygen uptake and work output in well-trained cyclists. Eur J Appl Physiol, 116(8), 1495-1502.
Kumar, P., & Bin-Jaliah, I. (2007). Adequate stimuli of the carotid body: more than an oxygen sensor? Respir Physiol Neurobiol, 157(1), 12-21.
Lorenzo, S., & Babb, T. G. (2013). Ventilatory responses at peak exercise in endurance-trained obese adults. Chest, 144(4), 1330-1339.
Luo, B. B., Yang, Y., Nieman, D. C., Zhang, Y. J., Wang, J., Wang, R., & Chen, P. J. (2013). A 6-week diet and exercise intervention alters metabolic syndrome risk factors in obese Chinese children aged 11-13 years. Journal of Sport and Health Science, 2(4), 236-241.
Maciejczyk, M., Szymura, J., Gradek, J., Cempla, J., & Wiecek, M. (2014). Physiological response is similar in overweight and normoweight boys during cycling: a longitudinal study. Acta Physiol Hung, 101(2), 236-249.
Nourry, C., Deruelle, F., Guinhouya, C., Baquet, G., Fabre, C., Bart, F., Mucci, P. (2005). High-intensity intermittent running training improves pulmonary function and alters exercise breathing pattern in children. Eur J Appl Physiol, 94(4), 415-423.
Pansayad, W. (2012). Obesity in working age. Academic Journal Institute of Physical Education, 4(1), 165 - 174.
Plowman., S. A., & Smith., D. L. (2008). Exercise physiology for health, fitness, and performance. Philadelphia, Pa. : Wolters Kluwer/Lippincott Williams & Wilkins.
Powers., S. K., & Howley., E. T. (2015). Exercise physiology : theory and application to fitness and performance. New York: McGraw-Hill.
Salome, C. M., King, G. G., & Berend, N. (2010). Physiology of obesity and effects on lung function. J Appl Physiol (1985), 108(1), 206-211.
Sharp, J. T., Henry, J. P., Sweany, S. K., Meadows, W. R., & Pietras, R. J. (1964). The Total Work of Breathing in Normal and Obese Men. J Clin Invest, 43, 728-739.
Susan A. Goldstein, Charles Weissman, Jeffrey Askanazi, Michael Rothkopf, J. Milic-Emili, & Kinney, J. M. (1987). Metabolic and ventilatory responses during very low level exercise. Clinical Science, 73(4), 417-424.
Tawonrungrojn, S. (2011). Indicators and Their Range of Values to Indicate Obesity. Songkla Med J, 9(2), 89-96.
Wongkritpetch, T. (2012). Physiology of Exercise. Bangkok: Tiranasan.
Yodit, C. (2010). Thai Boxing The Encyclopedia of Thai Youth Volume 35 (pp. 243-250). Bangkok: Dan Sutha Printing.