EFFECTS OF SUSTAINED MAXIMUM INSPIRATION VERSUS BALLOON-BLOWING BREATHING EXERCISE ON PULMONARY FUNCTION IN SCHOOL-AGE CHILDREN WITH ASTHMA
Main Article Content
Abstract
Purpose : The purpose of the study was to investigate the effects of sustained maximal inspiration and balloon blowing breathing exercise on pulmonary function in school-age children with asthma.
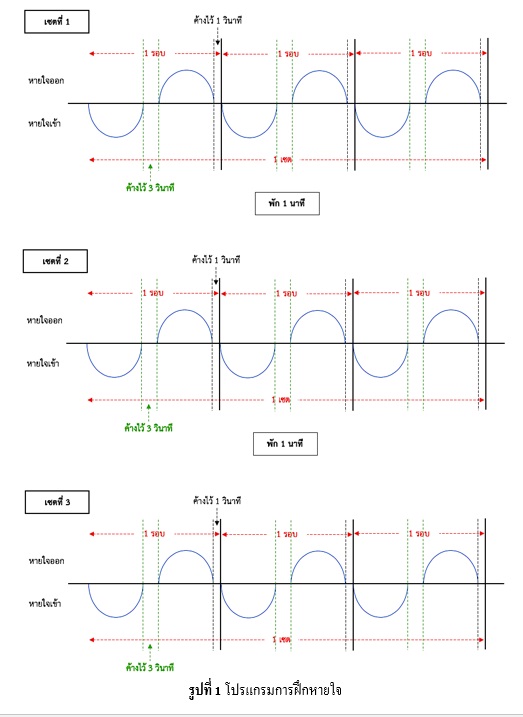
Methods : Sample of 30 school-age children with asthma, aged 7-12 years old, who visited at the outpatient department, Phramongkutklao Hospital, were recruited and randomly divided into 2 groups. The first group (n = 15) trained with sustained maximal inspiration (SMI) breathing exercise while the second group (n = 15) training with balloon-blowing breathing exercise. Participants were required to complete breathing exercise 5 times per week for the consecutive of 8 weeks. Physiological characteristics and pulmonary function variables were measured before and after training. The dependent variables were analyzed by paired t-test andindependent sample t-test. Differences were considered to be significant at p < .05.
Results : The results indicated that there were no significant differences in physiological data such as body weight, height, resting heart rate, systolic blood pressure, and diastolic blood pressure between before and after 8-week training in both groups. In addition, after training, the forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), peak expiratory flow, and maximum voluntary ventilation (MVV) in balloon-blowing breathing exercise group were significantly higher than the pre-test (p < .05), with no significant differences observed in the sustained maximal inspiration (SMI) breathing exercise group, except for higher maximum voluntary ventilation (MVV) (p < .05). No significant changes in all variables were found between two groups.
Conclusion : The present findings demonstrated that 8 weeks of balloon-blowing breathing exercise had more beneficial effects on pulmonary function compared to SIM in school-age children with asthma.
Article Details
References
Aekplakorn, W. (2014). The report of Thailand population health examination survey V. Health systems research institute.
Alexander Moeller., et al. (2015). Monitoring asthma in childhood: lung function, bronchial responsiveness and inflammation. Eur Respir Rev (24), 204–215.
Benjaponpitak S. (2012). Allergies in Children: Causes and Preventions. Nonthaburi: Beyond Enterprises.
Boonsawat, W. (2549). Problems of asthma treatment. Thai Journal of Tuberculosis Chest Diseases and Critical Care, 233-234.
Boonyaleepan S., and Boonyaleepan C. (2016). Unabridge edition of Allergies. (15th edition). Bangkok: Amarin Health Amarin Printing and Publishing.
Slader, C. A., Reddel, H. K., Spencer, L. M., Belousova, E. G., Armour, C. L., Bosnic- Anticevich, S. Z., Jenkins, C. R. (2006). Double blind randomised controlled trial of two different breathing techniques in the management of asthma. Thorax, 61, 651-656.
Collins, J. E., Gill, T. K., Chittleborough, C. R., Martin, A. J., Taylor, A. W., and Winefield, H. (2008). Mental, emotional, and social problems among school children with asthma. Journal of Asthma 45(6), 489-493.
Das, Nayak and Pradhan. (2018). Effect of Balloon Therapy vs. Bubble Therapy on LRTI among 3-12 Years Children. International Journal of Health Sciences & Research, 8, 144-147.
Dipti Agarwal., Prem Parkash Gupta., and Sushma Sood. (2017). Improvement in pulmonary functions and clinical parameters due to addition of breathing exercises in asthma patients receiving optimal treatment. Indian Journal of Allergy, Asthma and Immunology, 31, 61-68.
Global Initiative for Asthma. (2020). Global Strategy for Asthma Management and Prevention (2020 update). (Online). Retrieved July 8, 2020, from ginasthma Website: https://ginasthma.org/wp-content/uploads/ 2020/04/Main-pocket-guide_2020_04_03-final-wms.pdf
Hockenberry, M. J., and Wilson, D. (2015). Wong’s Nursing Care of Infant and Children (10th ed.). St. Louis and New York: ELSEVIER Health Sciences.
Hyun-Ju Jun., Ki-Jong Kim., Ki-Won nam., and CHang-Heon Kim. (2016). Effects of breathing exercises on lung capacity and muscle activities of elderly smokers. The Journal of Physical Therapy Science, 28, 1681-1685.
Jin-seop Kim., and Yeon-seop Lee. (2012). Effects of a Balloon-Blowing Exercise on Lung Function of Young Adult Smokers.J. Phys. Ther. Sci, 24, 531-534.
KyoChul Seo., and MiSuk Cho. (2018). The effects of a balloon-blowing exercise in a 90/90 bridge position using a ball on the pulmonary function of females in their twenties. The Journal of Physical TherapyScience, 30, 1267-1270.
Lee SC., et al. (2011) The effects of balloon blowups and upper abdominal exercise on respiratory rehabilitation. J Kor Phys Ther Sci, 18, 17–24 .
Lozier, M. J., Zahran, H. S., and Bailey, C. M. (2019). Assessing health outcomes, quality of life, and healthcare use among school-age children with asthma. Journal of Asthma, (56), 42-49.
Lumnoi, U., and Uakit, N. (2009). The effect of perceived self-efficacy program on self-management behavior among school-age children with asthma. Thai pediatric journal, 16(2), 108-121.
Mike Thomas., Anne Bruton. (2014). Breathing exercises for asthma. Breathe, 10(4), 313-322.
Niyomwit, K. (2017). Nursing Care for Ill Children with Acute Asthmatic Attack. Journal of Phrapokklao Nursing College, 28(1), 149-160.
Poachanukoon, O. and Chansakulporn, S. (2015). Children with Allergic Respiratory Diseases. Phra Nakhon Si Ayutthaya: Tienwattana Printing.
Ruanglapanun, W., Wichiencharoen, K., Seeda, R., Wannapong S. (2009). Impacts of Asthma Disease on School-age Asthmatic Children and Family. J Nurs Sci, 27(2), 18-27.
Sears M.R. (2007). Lung function decline in asthma. European Respiratory Journal (30), 411-413.
Sreedevi, R K. (2015). Effectiveness of balloon blowing on respiratory parameters among children with lower respiratory tract infection in selected hospitals, Kanyakumari District. Masters thesis, St. Xavier’s Catholic College of Nursing, Nagercoil.
Tangpathomwong, C., Nookong, A., and Senasuttipan, W. (2016). Children and Caregiver Factors Predicting Asthma Control of School Aged Children. Journal of Nursing and Health Care, 34(2), 67-76.
Tarun Saxena. and Manjari Saxena. (2009). The effect of various breathing exercises (pranayama) in patients with bronchial asthma of mild to moderate severity. Int J Yoga, 22–25.
Thaneesap K. (2017). Breathing Practices: Easy and Beneficial more than you think. In Siriraj Medical Record, 10(2), 122-125.
The Global Asthma Network. (2018). The Global Asthma Report 2018. (Online). Retrieved September 3, 2018, from Global Asthma Network Website: http://globalasthmareport.org/Global%20Asthma% 20Report%202018.pdf
Walker, T. J., and Reznik, M. (2014). In-school asthma management and physical activity: children’s perspectives. Journal of Asthma 51(8), 808-813.
Woodruff G., Bhakta R., and Fahy V. ASTHMA: PATHOGENESIS AND PHENOTYPES. In editor-in-chief, V. Courtney Broaddus; editors, Robert J. Mason, Joel D. Ernst,
Talmadge E. King Jr., Stephen C. Lazarus, John F. Murray, Jay A. Nadel, Arthur S. Slutsky; thoracic imaging editor, Michael B. Gotway., (2016). Murray & Nadel’s Textbook of Respiratory Medicine, pp.713-730. Canada,
Yimliang S., Rattanavichai P. and Chuckvichai C. (2009). Treating Asthma in Children technique development by Multidisciplinary Team of Pichit Hospital. In Journal of Nursing Division, 36(3), 96-112.