The scalp nodules as the presenting symptom of primary localized cutaneous nodular amyloidosis:A rare case report
Keywords:
nodular amyloidosis, primary localized cutaneous amyloidosis, scalp nodulesAbstract
BORRIBOON T, SAHAKARO C, SAWASDIPONG J, SUDTIKOONASETH P. THE SCALP NODULES AS THE PRESENTING SYMPTOM OF PRIMARY LOCALIZED CUTANEOUS NODULAR AMYLOIDOSIS: A RARE CASE REPORT. THAI J DERMATOL 2020;36:67-72.
INSTITUTE OF DERMATOLOGY, DEPARTMENT OF MEDICAL SERVICES, MINISTRY OF PUBLIC HEALTH, BANGKOK, THAILAND.
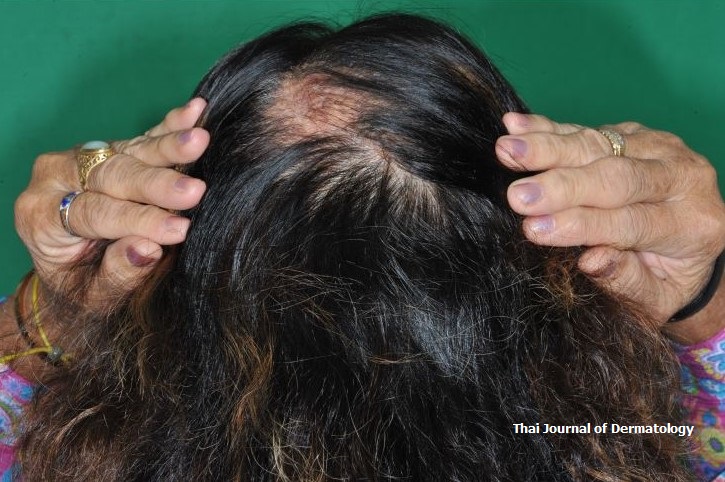
Primary localized cutaneous nodular amyloidosis (PLCNA) is a rare variant of primary cutaneous amyloidosis which is characterized by a single or multiple yellowish waxy nodule with telangiectasias. The predilection site is the acral area but there are some reports presenting on the head and neck regions. Amyloid protein deposition in nodular amyloidosis originates from immunoglobulin light chains secreted by plasma c ells infiltrating the skin. We hereby report a case of 68-year-old women presented with multiple
waxy skin-colored to yellowish nodules on the scalp for 2 years which prior suspected of nevus sebaceous. The incisional biopsy was done.
Histopathologic findings revealed nodular deposits of amorphous eosinophilic material in the entire dermis. The Congo red stain was positive for amyloid. The patient underwent exhaustive systemic evaluations, which were all negative. According to these finding, the diagnosis of primary localized cutaneous nodular amyloidosis was made. The patient was advised to undergo long term follow-up to monitor for potential progression to systemic disease.
References
Lachmann HJ, Hawkins PN. Amyloidosis of the skin. In: Goldsmith LA, Gilchrest BA, Paller AS, Leffel DJ, Wolff K, editors. Fitzpatrick’s dermatology of general medicine. 8thed. New York: Mcgraw-Hill 2012:1574-83.
Meijer JM, Schonland SO, Palladini G, et al. Sjogren’s syndrome and localized nodular cutaneous amyloidosis. Arthritis Rheum 2008;58:1992-9.
Groves RW. Amyloidosis. In: Bolognia JL, Schaffer JV, Cerroni L, editors. Dermatology. 4th ed. China: Elsevier 2018;754-63.
Lee DY, Kim YJ, Lee JY, Kim MK, Yoon TY. Primary localized cutaneous nodular amyloidosis following local trauma. Ann Dermatol 2011;23:515-8.
Schwendiman MN, Beachkofsky TM, Wisco OJ, Owens NM, Hodson DS. Primary cutaneous nodular amyloidosis: case report and review of the literature. Cutis 2009; 84: 87-92.
Mehrotra K, Dewan R, Kumar JV, Dewan A. Primary cutaneous amyloidosis: a clinical, histopathological and immunofluorescence study. J Clin Diagn Res 2017;11:1-5.
Trignano E, Ciudad P, Fallico N, Chen H-C. Nodular cutaneous amyloidosis of the scalp reconstructed with a free anterolateral thigh flap: a case report. J Oral Maxillofac Surg 2012;70:e481–3.
Yoneyama K, Tochigi N, Oikawa A, Shinkai H, Utani A. Primary localized cutaneous nodular amyloidosis in a patient with Sjögren’s syndrome: a review of the literature. J Dermatol 2005;32:120–3.
Lien MH, Railan D, Nelson BR. The efficacy of dermabrasion in the treatment of nodular amyloidosis. J Am Acad Dermatol 1997; 36: 315-6.
Alster TS, Manaloto RM. Nodular amyloidosis treated with a pulsed dye laser. Dermatol Surg 1999;25:133–5.
Raymond J, Choi J. Nodular cutaneous a myloidosis effectively treated with intralesional methotrexate. J Am Acad Dermatol 2016;2:373-6.
Hirschfield GM, Hawkins PN. Amyloidosis: new strategies for treatment. Int J Biochem Cell Biol 2003;35:1608-13.
Pepys MB, Herbert J, Hutchinson WL, et al. Targeted pharmacological depletion of serum amyloid P component for treatment of human amyloidosis. Nature 2002;417:254-9.
Downloads
Published
How to Cite
Issue
Section
License
เนื้อหาและข้อมูลในบทความที่ลงตีพิมพ์ในวารสารโรคผิวหนัง ถือเป็นข้อคิดเห็นและความรับผิดชอบของผู้เขียนบทความโดยตรงซึ่งกองบรรณาธิการวารสาร ไม่จำเป็นต้องเห็นด้วย หรือร่วมรับผิดชอบใดๆ
บทความ ข้อมูล เนื้อหา รูปภาพ ฯลฯ ที่ได้รับการตีพิมพ์ในวารสารโรคผิวหนัง ถือเป็นลิขสิทธิ์ของวารสารฯ หากบุคคลหรือหน่วยงานใดต้องการนำทั้งหมดหรือส่วนหนึ่งส่วนใดไปเผยแพร่ต่อหรือเพื่อกระทำการใดๆ จะต้องได้รับอนุญาตเป็นลายลักอักษรจากบรรณาธิการวารสารโรคผิวหนังก่อนเท่านั้น


