Correlation between quality of life assessed by Thai-version of Skindex-29 scores and disease severity among patients with pemphigus
Keywords:
Quality of life, skindex-29, pemphigusAbstract
Background: Pemphigus is an autoimmune blistering disease which has a great negative impact on the quality of life (QOL) in many aspects, such as physical, psychological and social status. Exploring associated factors might be beneficial and improve the QOL.
Objective: To examine the correlation between Pemphigus Disease Area Index (PDAI) score and Thai-version of Skindex-29 score in pemphigus and define other variable factors which affected the QOL.
Materials and Methods: Fifty-nine pemphigus patients at the Institute of Dermatology in Thailand from July 2017 to September 2017 were enrolled. The QOL was evaluated by the Thai-version of Skindex-29. The clinical severity was assessed by PDAI scoring system. Correlation analysis was used to evaluate the correlation between Skindex-29 and PDAI scores.
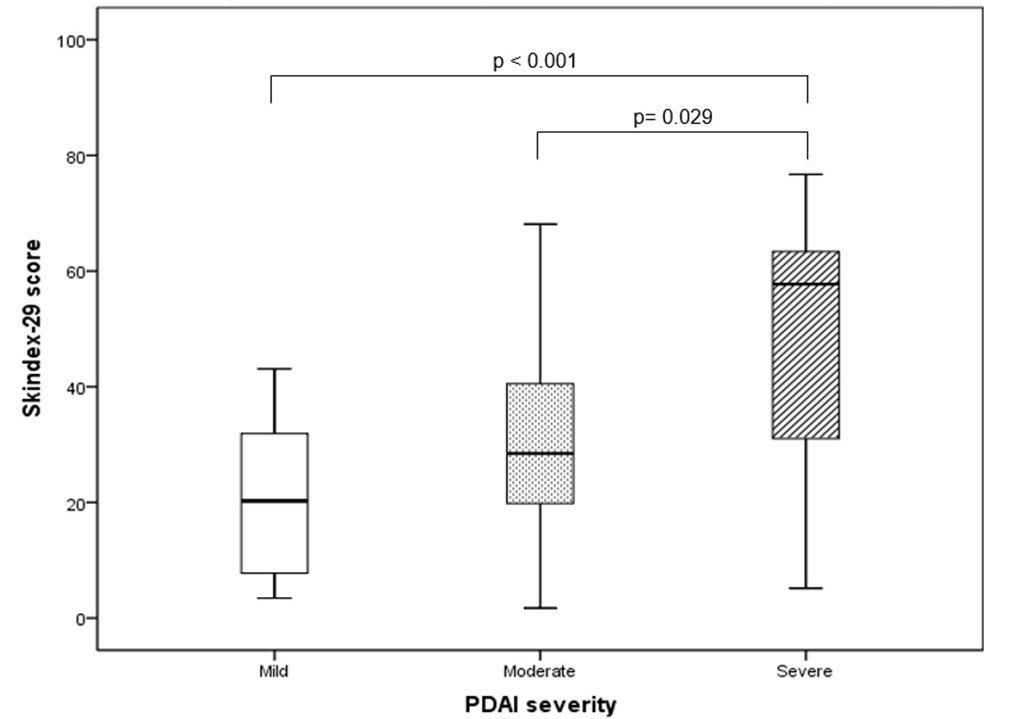
Result: The disease severity scores assessed by PDAI had a low positive correlation with the Skindex-29 scores (r = 0.387, P = 0.002). Furthermore, the younger age group was significantly associated with lower QOL (odds ratio [OR], 0.923; 95% confidence interval [CI], 0.866 to 0.984; P = 0.013). Shorter duration of disease showed higher risk of poorer QOL in emotion (OR, 11.752; 95% CI, 1.093 to 126.285; P = 0.042) and functioning scores (OR, 22.131; 95% CI, 2.117 to 231.317; P = 0.010).
Conclusion: Our study demonstrated a significant negative effect on the QOL in pemphigus assessed by Thai-version of Skindex-29 score. The clinical severity, age and duration of the disease were important factors associated with poor QOL.
References
Chams-Davatchi C, Valikhani M, Daneshpazhooh M, et al. Pemphigus: analysis of 1209 cases. Int J Dermatol 2005;44:470-6.
Regier DA, Boyd JH, Burke JD, Jr, et al. One-month prevalence of mental disorders in the United States. Based on five Epidemiologic Catchment Area sites. Arch Gen Psychiatry 1988;45:977-86.
Paradisi A, Sampogna F, Di Pietro C, et al. Quality-of-life assessment in patients with pemphigus using a minimum set of evaluation tools. J Am Acad Dermatol 2009;60:261-9.
Penha MA, Farat JG, Miot HA, Barraviera SR. Quality of life index in autoimmune bullous dermatosis patients. An Bras Dermatol 2015;90:190-4.
Sung JY, Roh MR, Kim S-C. Quality of Life Assessment in Korean Patients with Pemphigus. Annals of Dermatology 2015;27:492-8.
Tantanasrigul P, Sudtikoonaseth P, Vejjabhinanta V, Kattipathanapong P. Thai version Skindex-29 validation test among patients with cutaneous lupus erythematosus and pemphigus. Unpublished.
Chren MM, Lasek RJ, Quinn LM, Mostow EN, Zyzanski SJ. Skindex, a quality-of-life measure for patients with skin disease: reliability, validity, and responsiveness. J Invest Dermatol 1996;107:707-13.
Daniel BS, Hertl M, Werth VP, Eming R, Murrell DF. Severity score indexes for blistering diseases. Clin Dermatol 2012;30:108-13.
Rahbar Z, Daneshpazhooh M, Mirshams-Shahshahani M, et al. Pemphigus disease activity measurements: pemphigus disease area index, autoimmune bullous skin disorder intensity score, and pemphigus vulgaris activity score. JAMA Dermatol 2014;150:266-72.
Zhao CY, Murrell DF. Outcome measures for autoimmune blistering diseases. J Dermatol 2015;42:31-6.
Grover S. Scoring systems in pemphigus. Indian J Dermatol 2011;56:145-9.
Murrell DF, Dick S, Ahmed AR, et al. Consensus statement on definitions of disease, end points, and therapeutic response for pemphigus. J Am Acad Dermatol 2008;58:1043-6.
Shimizu T, Takebayashi T, Sato Y, et al. Grading criteria for disease severity by pemphigus disease area index. J Dermatol 2014;41:969-73.
Chren MM, Lasek RJ, Flocke SA, Zyzanski SJ. Improved discriminative and evaluative capability of a refined version of Skindex, a quality-of-life instrument for patients with skin diseases. Arch Dermatol 1997;133:1433-40.
Both H, Essink-Bot ML, Busschbach J, Nijsten T. Critical review of generic and dermatology-specific health-related quality of life instruments. J Invest Dermatol 2007;127:2726-39.
Augustin M, Wenninger K, Amon U, et al. German adaptation of the Skindex-29 questionnaire on quality of life in dermatology: validation and clinical results. Dermatology 2004;209:14-20.
Jones-Caballero M, Penas PF, Garcia-Diez A, Badia X, Chren MM. The Spanish version of Skindex-29. Int J Dermatol 2000;39:907-12.
Janowski K, Steuden S, Bereza B. The Polish version of Skindex-29: psychometric properties of an instrument to measure quality of life in dermatology. Postepy Dermatol Alergol 2014;31:12-20.
Aksu AE, Urer MS, Sabuncu I, Saracoglu ZN, Chren MM. Turkish version of Skindex-29. Int J Dermatol 2007;46:350-5.
Prinsen CA, Lindeboom R, Sprangers MA, Legierse CM, de Korte J. Health-related quality of life assessment in dermatology: interpretation of Skindex-29 scores using patient-based anchors J Invest Dermatol. 2010;130:1318-22.
Hinkle DE, Wiersma W, Jurs SG. Applied statistics for the behavioral sciences. 5th ed. Boston: Houghton Mifflin; 2003.
Sebaratnam DF, McMillan JR, Werth VP, Murrell DF. Quality of life in patients with bullous dermatoses. Clin Dermatol 2012;30:103-7.
Hagen SL, Grey KR, Korta DZ, Kelly KM. Quality of life in adults with facial port-wine stains. J Am Acad Dermatol 2017;76:695-702.
Downloads
Published
How to Cite
Issue
Section
License
เนื้อหาและข้อมูลในบทความที่ลงตีพิมพ์ในวารสารโรคผิวหนัง ถือเป็นข้อคิดเห็นและความรับผิดชอบของผู้เขียนบทความโดยตรงซึ่งกองบรรณาธิการวารสาร ไม่จำเป็นต้องเห็นด้วย หรือร่วมรับผิดชอบใดๆ
บทความ ข้อมูล เนื้อหา รูปภาพ ฯลฯ ที่ได้รับการตีพิมพ์ในวารสารโรคผิวหนัง ถือเป็นลิขสิทธิ์ของวารสารฯ หากบุคคลหรือหน่วยงานใดต้องการนำทั้งหมดหรือส่วนหนึ่งส่วนใดไปเผยแพร่ต่อหรือเพื่อกระทำการใดๆ จะต้องได้รับอนุญาตเป็นลายลักอักษรจากบรรณาธิการวารสารโรคผิวหนังก่อนเท่านั้น


