Effect of Different Shampoos and Contact Time on Microsporum canis Infected Hair: In vitro Model Study
Keywords:
Tinea capitis, Microsporum canis, zinc pyrithione shampoo, selenium sulfideAbstract
Background: Tinea capitis is commonly caused by Microsporum canis. The standard treatment is systemic antifungal medications with adjunctive use of an antifungal shampoo. The current information about the effect of shampoos is limited.
Objectives: To compare the effects of different shampoos and contact times on M. canis infected hair.
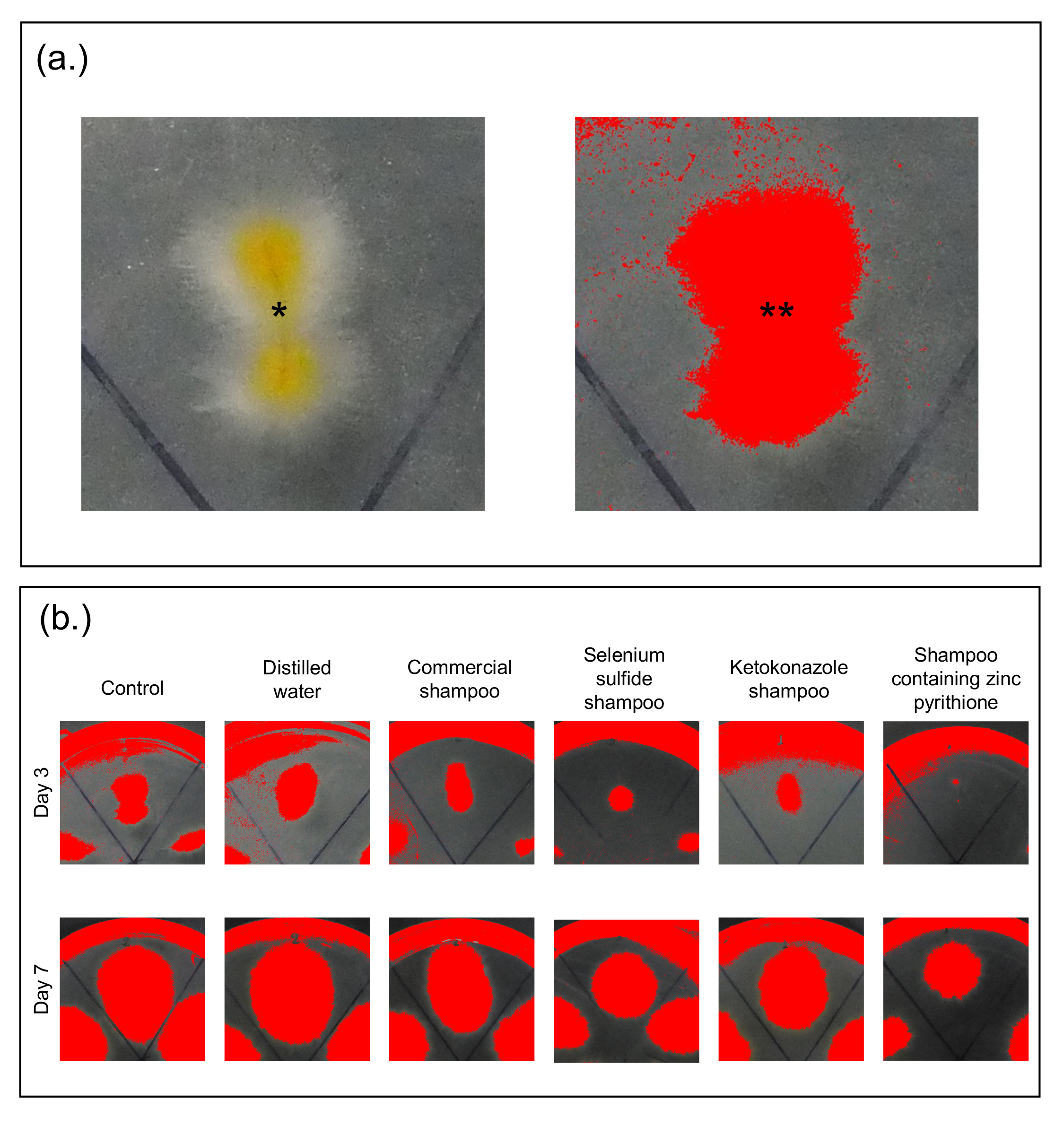
Methods: This in vitro study was conducted at the Mycology Laboratory in a tertiary hospital, Thailand, in 2020. Hair taken from a child was disinfected and incubated with an M. canis colony for 15 days before divided into ten groups. Each of these samples was then mixed with distilled water, a commercial shampoo, a ketoconazole shampoo, a selenium sulfide shampoo, or a zinc pyrithione shampoo for either 2 or 5 minutes. Those samples and control-group samples were cultured for 7 days before fungal growth areas were collected and analyzed.
Results: At Day 3, the fungal colony growth areas on the samples mixed with commercial shampoo, ketoconazole shampoo, selenium sulfide shampoo, and zinc pyrithione shampoo were significantly smaller than that of the control. Moreover, the samples mixed with ketoconazole shampoo, selenium sulfide shampoo, and zinc pyrithione shampoo demonstrated a statistically different fungal-growth area from the control at Day 7. However, the duration of mixing resulted in similar areas of fungal growth for all samples.
Conclusions: Shampoos containing zinc pyrithione and commercial shampoos are alternative adjunctive treatments for tinea capitis arising from M. canis. In addition, contact with the shampoos for at least 5 minutes appears to be optimal.
References
Fuller LC, Barton RC, Mohd Mustapa MF, Proudfoot LE, Punjabi SP, Higgins EM. British Association of Dermatologists' guidelines for the management of tinea capitis 2014. Br J Dermatol 2014;171:454-63.
Mayser P, Nenoff P, Reinel D, et al. S1 guidelines: Tinea capitis. J Dtsch Dermatol Ges 2020;18:161-79.
Ungpakorn R. Mycoses in Thailand: current concerns. Nihon Ishinkin Gakkai Zasshi 2005;46:81-6.
Bunyaratavej S, Leeyaphan C, Rujitharanawong C, Muanprasat C, Matthapan L. Clinical and Laboratory Characteristics of a Tinea Capitis Outbreak Among Novice Buddhist Monks. Pediatr Dermatol 2017;34:371-3.
Chan YC, Friedlander SF. Therapeutic options in the treatment of tinea capitis. Expert Opin Pharmacother 2004;5:219-27.
Moriello KA. In vitro efficacy of shampoos containing miconazole, ketoconazole, climbazole or accelerated hydrogen peroxide against Microsporum canis and Trichophyton species. J Feline Med Surg 2017;19:370-4.
Salkin IF, Hollick GE, Hurd NJ, Kemna ME. Evaluation of human hair sources for the in vitro hair perforation test. J Clin Microbiol 1985;22:1048-9.
Gupta AK, Mays RR, Versteeg SG, et al. Tinea capitis in children: a systematic review of management. J Eur Acad Dermatol Venereol 2018;32:2264-74.
Martinez-Rossi NM, Peres NT, Rossi A. Pathogenesis of Dermatophytosis: Sensing the Host Tissue. Mycopathologia 2017;182:215-27.
Trüeb RM. Shampoos: ingredients, efficacy and adverse effects. J Dtsch Dermatol Ges 2007;5:356-65.
Reeder NL, Xu J, Youngquist RS, Schwartz JR, Rust RC, Saunders CW. The antifungal mechanism of action of zinc pyrithione. Br J Dermatol 2011;165:9-12.
Chen C, Koch LH, Dice JE, et al. A randomized, double-blind study comparing the efficacy of selenium sulfide shampoo 1% and ciclopirox shampoo 1% as adjunctive treatments for tinea capitis in children. Pediatr Dermatol 2010;27:459-62.
Greer DL. Successful treatment of tinea capitis with 2% ketoconazole shampoo. Int J Dermatol 2000;39:302-4.
Committee on Infectious Diseases, American Academy of Pediatrics. Red Book [Electronic Resource]: 2015 Report of the Committee on Infectious Diseases/Committee on Infectious Diseases, American Academy of Pediatrics, 13th edn. American Academy of Pediatrics, Elk Grove Village, Illinois, 2015.
Downloads
Published
How to Cite
Issue
Section
License
เนื้อหาและข้อมูลในบทความที่ลงตีพิมพ์ในวารสารโรคผิวหนัง ถือเป็นข้อคิดเห็นและความรับผิดชอบของผู้เขียนบทความโดยตรงซึ่งกองบรรณาธิการวารสาร ไม่จำเป็นต้องเห็นด้วย หรือร่วมรับผิดชอบใดๆ
บทความ ข้อมูล เนื้อหา รูปภาพ ฯลฯ ที่ได้รับการตีพิมพ์ในวารสารโรคผิวหนัง ถือเป็นลิขสิทธิ์ของวารสารฯ หากบุคคลหรือหน่วยงานใดต้องการนำทั้งหมดหรือส่วนหนึ่งส่วนใดไปเผยแพร่ต่อหรือเพื่อกระทำการใดๆ จะต้องได้รับอนุญาตเป็นลายลักอักษรจากบรรณาธิการวารสารโรคผิวหนังก่อนเท่านั้น


