A Case Report of Papulonodular Mucinosis Associated with Unclassified Autoimmune Connective Tissue Disease
Keywords:
Papulonodular mucinosis, autoimmune connective tissue diseasesAbstract
Papulonodular mucinosis (PNM) is an uncommon but distinctive cutaneous manifestation of autoimmune connective tissue disease mainly associated with lupus erythematosus. Mucin deposition in the dermis is a common histologic finding. The pathogenesis is still uncertain but it is thought to be due to increased glycosaminoglycans production by dermal fibroblast stimulated by some cytokines or immunoglobulins. In terms of treatment, PNM is usually unsatisfactory. Many modalities have been suggested including glucocorticosteroids (topical, intralesional or systemic), antimalarial agents, retinoids, cyclophosphamide, methotrexate, plasmapheresis or surgical procedures such as laser and excision may have benefits.
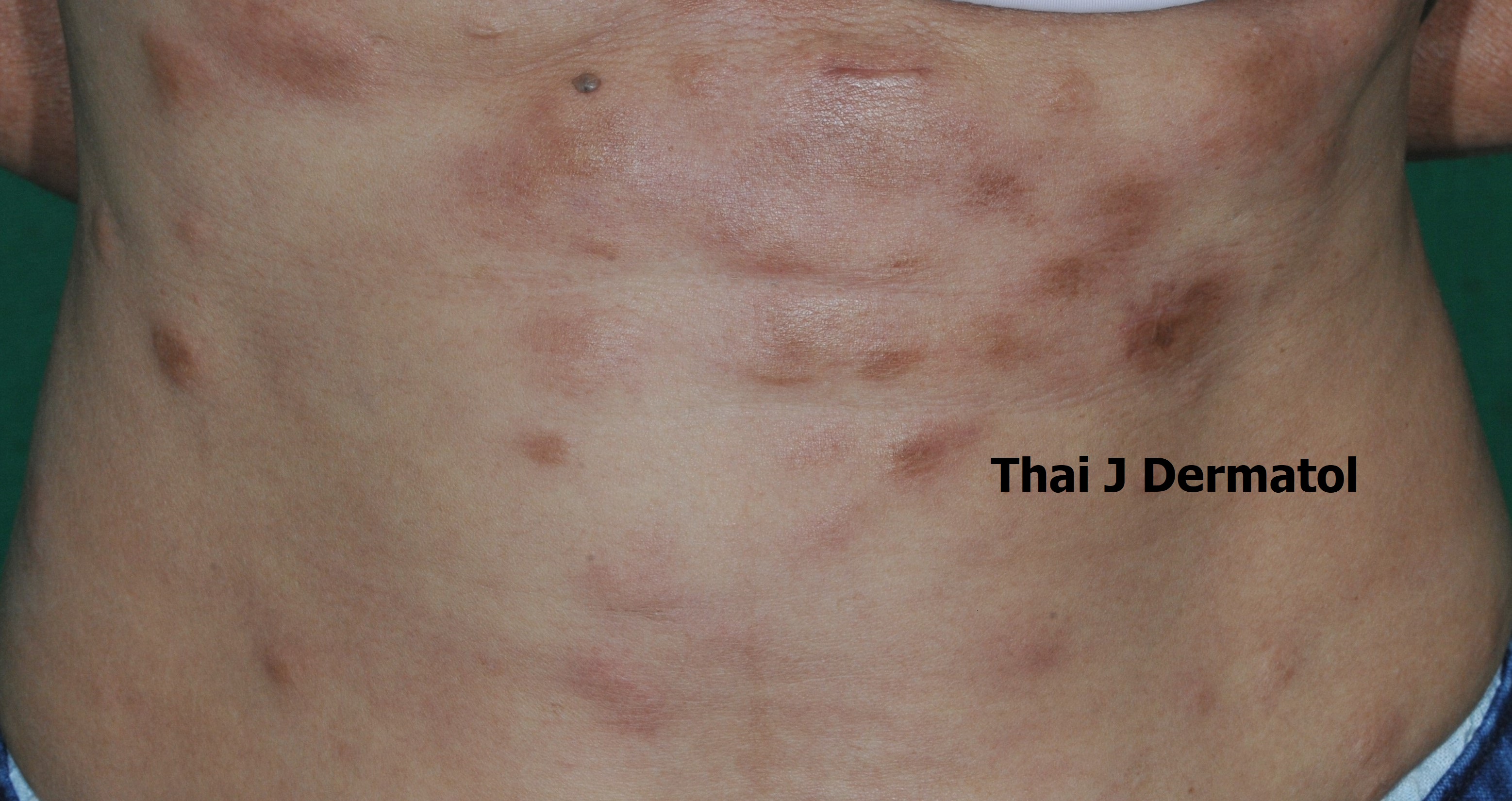
We report a case of 45-year-old female presented with a 5-years history of multiple erythematous hyperpigmented papules, nodules on trunk and skin colored papules coalescing to plaques on both forearms and knuckles. The patient denied systemic symptoms and the physical examination showed only Raynaud phenomenon. The histopathology and special staining were compatible with dermal mucinosis. Laboratory investigation showed high titer antinuclear antibodies and weakly positive anti-Jo1 while other serological tests for autoimmune disease were normal. The final diagnosis of papulonodular mucinosis associated with unclassified autoimmune connective tissue disease (AI-CTDs) was made as there was neither symptom nor laboratory result of definite AI-CTDs. Clinical improvement was seen after 3 months of oral methotrexate and topical glucocorticoids.
References
Rongioletti F, Rebora A. The new cutaneous mucinoses: A review with an up-to-date classification of cutaneous mucinoses. J Am Acad Dermatol 1991;24:265-70.
Rongioletti F, Bolognia JL, Schaffer JV, Cerroni L. Dermatology. 4th ed. Elsevier Spain: Mucinoses; 2018;742–53.
Gold SC. An unusual popular eruption associated with lupus erythematosus. Br J Dermatol 1954;66:429-33.
Rongioletti F, Rampini P, Parodi A, Rebora A. Papular mucinosis associated with generalized morphea. Br J Dermatol 1999;141:905-8.
Van Zander J, Shaw JC. Papular and nodular mucinosis as a presenting sign of progressive systemic sclerosis. J Am Acad Dermatol 2002;46:304–6.
Sonntag M, Lehmann P, Megahed M, Ruzicka T, Kuhn A. Papulonodular mucinosis associated with subacute cutaneous lupus erythematosus. Dermatology 2003;206:326-9.
Lee WS, Chung J, Ahn SK. Plaque and postauricular nodular mucinosis associated with lupus erythematosus. Int J Dermatol 1997;36: 356-73.
Gouveia Al, Sousa M, Osório-Valente R, et al. Papulonodular mucinosis an unusual presenting feature of systemic lupus erythematosus. International journal of dermatology 2016;55:e607-8.
Pandya AG, Sontheimer RD, Cockerell CJ, Takashima A, Piepkorn M. Papulonodular mucinosis associated with systemic lupus erythematosus: possible mechanisms of increased glycosaminoglycan accumulation. J Am Acad Dermatol 1995;32:199-205.
Rongioletti F, Parodi A, Rebora A. Papular and nodular mucinosis as a sign of lupus erythematosus. Dermatologica 1990;180:221-23
Ortize VG, Krishnan RS, Chen LL, Hsu S. Papulonodular mucinosis in systemic lupus erythematosus. Dermatol Online J 2004;10:16
Lowe L, Rapini RP, Golitz LE, Johnson TM. Papulonodular dermal mucinosis in lupus erythematosus. J Am Acad Dermatol 1992;27:312-5.
Dreier B, Hammad-Zulfoghari D, Beiteke U, Frosch PJ: Papulöse Muzinose: Erfolgreiche Therapie mit Plasmapherese. Hautarzt 1997;48:648–52.
Maruyama M, Miyauchi S, Hashimoto K. Massive cutaneous mucinosis associated with systemic lupus erythematosus. Br J Dermatol 1997;137:450-3.
Downloads
Published
How to Cite
Issue
Section
License
เนื้อหาและข้อมูลในบทความที่ลงตีพิมพ์ในวารสารโรคผิวหนัง ถือเป็นข้อคิดเห็นและความรับผิดชอบของผู้เขียนบทความโดยตรงซึ่งกองบรรณาธิการวารสาร ไม่จำเป็นต้องเห็นด้วย หรือร่วมรับผิดชอบใดๆ
บทความ ข้อมูล เนื้อหา รูปภาพ ฯลฯ ที่ได้รับการตีพิมพ์ในวารสารโรคผิวหนัง ถือเป็นลิขสิทธิ์ของวารสารฯ หากบุคคลหรือหน่วยงานใดต้องการนำทั้งหมดหรือส่วนหนึ่งส่วนใดไปเผยแพร่ต่อหรือเพื่อกระทำการใดๆ จะต้องได้รับอนุญาตเป็นลายลักอักษรจากบรรณาธิการวารสารโรคผิวหนังก่อนเท่านั้น


