Exfoliative Dermatitis in Thai Children: 10 Years Review
Keywords:
Exfoliative dermatitis, children, neonateAbstract
Background: Exfoliative dermatitis is an uncommon, potentially serious skin condition. Thus it might poses a significant challenge to find the underlying etiologies.
Objective: To determine the etiologies, clinical presentations, laboratory findings and outcomes of exfoliative dermatitis in Thai children.
Material and methods: A retrospective study of patients diagnosed of exfoliative dermatitis at the Dermatology Unit, Queen Sirikit National Institute of Child Health during January 2009 to December 2019 was reviewed.
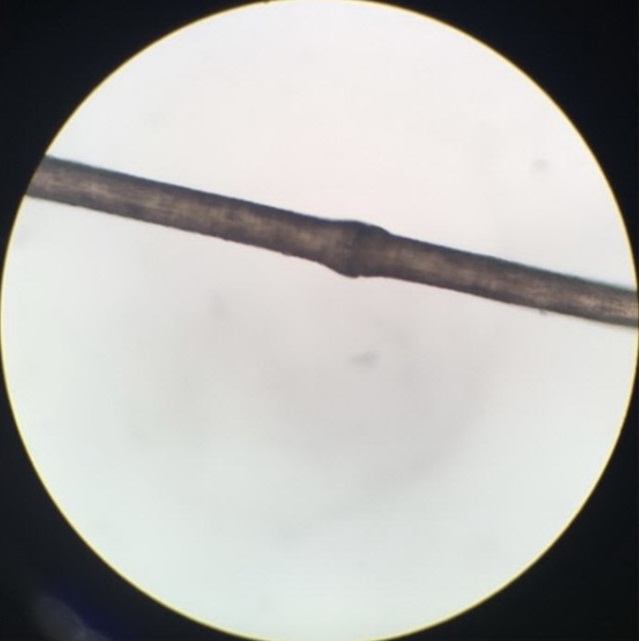
Results: Forty-one patients were identified. Age ranged from birth to12 years, with median age was 5 months (IQR 0-33 months), female to male ratio of 1:1. Clinical findings were pruritus (80.5%), fever (51.2%), failure to thrive (14.6%) and alopecia (12.2%). The most common causative diseases were inflammatory dermatoses in 26 cases (63.4%), including atopic dermatitis in 15 cases (36.6%), psoriasis in 8 cases (19.5%), pityriasis rubra pilaris in 2 cases (4.9%) and pityriasis lichenoides et varioliformis acuta in
1 case (2.4%). Other causes were genodermatoses in 9 cases (22.0%), primary immunodeficiency syndrome in 2 cases (4.9%), drug allergy in 1 case (2.4%) and unknown causes in 3 cases (7.3%). In neonatal exfoliative dermatitis (N=11), the underlying causes included congenital ichthyosis in 9 cases (81.8%) and Netherton syndrome in 2 cases (18.2%). Skin biopsies were done in 30 cases (73.2%). The follow up of 37 cases (90.2%) revealed good complete recovery in 8 patients (19.5%), chronic dermatoses in 19 patients (46.3%) and persistent exfoliative dermatitis in 10 patients (24.4%). Mortality rate was 2.4% due to severe sepsis.
Conclusion: The clinical features of exfoliative dermatitis are unspecified with few cause-orienting clues. Etiologies of exfoliative dermatitis depend on the patient’s age group. In neonatal exfoliative dermatitis are most commonly due to congenital ichthyosis or immunodeficiency syndrome. Likewise, exfoliative dermatitis with infants and childhood onset are most attributed to inflammatory dermatoses.
References
Hogan PA, Langley RGB. Papulosquamous disease. In Schachner L, Hansen R, eds. Pediatric Dermatology, 4th ed. U.S.A: Elsevier Limited 2011:901-51.
Whittaker S. Erythroderma. In: Bolognia JL, Schaffer J, Cerroni L, eds. Dermatology. 4th ed. U.S.A.: Elsevier Limited 2018:175-87.
Okoduwa C, Lambert WC, Schwartz RA, et al. Erythroderma: review of potentially life-threatening dermatosis. Indian J Dermatol 2009;54:1–6.
Boull CL, Hook K P. Neonatal erythroderma - clinical perspectives. Research and Reports in Neonatology 2017;7:1-9.
Dhar S, Banerjee R, Malakar R. Neonatal erythroderma: diagnostic and therapeutic challenges. Indian J Dermatol 2012;57:475-8.
Sehgal VN, Srivastava G. Erythroderma/generalized exfoliative dermatitis in pediatric practice: An overview. Int J Dermatol 2006;45:831-9.
Sarkar R, Garg VK. Erythroderma in children. Indian J Dermatol Venereol Leprol 2010;76:341-7.
Leenutaphong V, Kulthanan K, Pohboon C, Suthipinittharm P, Sivayathorn A, Sunthonpalin P. Erythroderma in Thai patients. J Med Assoc Thai 1999;82:743-8.
Li J, Zheng HY. Erythroderma: A clinical and prognostic study. Dermatology 2012;225:154-62.
Khaled A, Sellami A, Fazaa B, Kharfi M, Zeglaoui F, Kamoun MR. Acquired erythroderma in adults: A clinical and prognostic study. J Eur Acad Dermatol Venereol 2010; 24:781-8.
César A, Cruz M, Mota A, Azevedo F. Erythroderma. A clinical and etiological study of 103 patients. J Dermatol Case Rep 2016;10:1-9.
Pal S, Haroon TS. Erythroderma: A clinico-etiologic study of 90 cases. Int J Dermatol 1998;37:104-7.
Akhyani M, Ghodsi ZS, Toosi S, Dabbaghian H. Erythroderma: A clinical study of 97 cases. BMC Dermatol 2005;5:5.
Miyashiro D, Sanches JA. Erythroderma: a prospective study of 309 patients followed for 12 years in a tertiary center. Sci Rep 2020;10:9774.
Hulmani M, NandaKishore B, Bhat MR, et al. Clinico-etiological study of 30 erythroderma cases from tertiary center in South India. Indian Dermatol Online J 2014;525-9.
Al-Dhalimi MA. Neonatal and infantile erythroderma: A clinical and Follow-up study of 42 cases. J Dermatol 2007;34:302-7.
Pruszkowski A, Bodemer C, Fraitag S, Teillac-Hamel D, Amoric JC, de Prost Y. Neonatal and infantile erythrodermas: A retrospective study of 51 patients. Arch Dermatol 2000;136:875-80.
Sarkar R, Sharma RC, Koranne RV, Sardana K. Erythroderma in children: A clinico-etiological study. J Dermatol 1999;26:507-11.
Wisuthsarewong W, Nitiyarom R, Buddawong T, Exfoliative dermatitis in Thai children. Astrocyte 2017;3:184-7.
Kalsy J, Puri KJPS. Erythoderma in children: Clinico-etiological study from Punjab. Indian J Pediatr Dermatol 2013;14:9-12.
Simpson EL, Leung DYM, Eichenfield LF, Boguniewicz M. Atopic dermatitis. In: Kang S, Amagai M, Bruckner AL, et al., eds. Fitzpatrick’s dermatology 9th ed. New York: McGraw-Hill; 2019:363-84.
Rym BM, Mourad M, Bechir Z, et al. Erythroderma in adults: A report of 80 cases. Int J Dermatol 2005;44:731-5.
Downloads
Published
How to Cite
Issue
Section
License
เนื้อหาและข้อมูลในบทความที่ลงตีพิมพ์ในวารสารโรคผิวหนัง ถือเป็นข้อคิดเห็นและความรับผิดชอบของผู้เขียนบทความโดยตรงซึ่งกองบรรณาธิการวารสาร ไม่จำเป็นต้องเห็นด้วย หรือร่วมรับผิดชอบใดๆ
บทความ ข้อมูล เนื้อหา รูปภาพ ฯลฯ ที่ได้รับการตีพิมพ์ในวารสารโรคผิวหนัง ถือเป็นลิขสิทธิ์ของวารสารฯ หากบุคคลหรือหน่วยงานใดต้องการนำทั้งหมดหรือส่วนหนึ่งส่วนใดไปเผยแพร่ต่อหรือเพื่อกระทำการใดๆ จะต้องได้รับอนุญาตเป็นลายลักอักษรจากบรรณาธิการวารสารโรคผิวหนังก่อนเท่านั้น


