Identification if a New FLCN Variant in a Patient with Suspected Birt-Hogg-Dubé Syndrome Presented with Cutaneous Late-Onset Angiofibroma
Keywords:
Birt-Hogg-Dubé Syndrome, Missense Mutation, Angiofibroma, FLCN geneAbstract
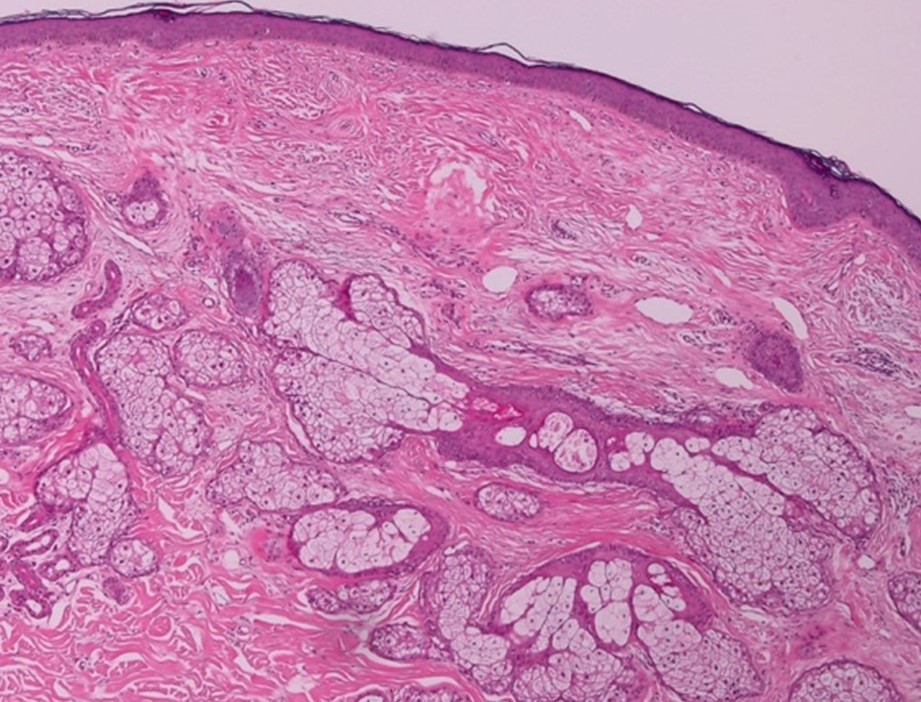
A 63-year-old female presented with a 40-year history of multiple skin-colored facial papules with previous medical history of two episodes of spontaneous pneumothorax at the age of 28 and 62 years. Multiple cysts in both lungs were detected by high-resolution computed tomography chest. Physical examination revealed multiple skin-colored facial papules on her nose and malar area. Sanger sequencing of FLCN showed a new heterozygous mutation, c.1448T>C, p.Leu483Pro, potentially resulting in abnormally functioning protein. Even in the absence of characteristic skin histology, the diagnosis was made using one major criterion (FLCN germline mutation) and one minor criterion (many lung cysts) in accordance with the European Birt-Hogg-Dubé Syndrome Consortium diagnostic criteria6
References
Nickerson ML, Warren MB, Toro JR, et al. Mutations in a novel gene lead to kidney tumors, lung wall defects, and benign tumors of the hair follicle in patients with Birt-Hogg-Dubé syndrome. Cancer Cell 2002;2:157-64.
Toro JR, Wei MH, Glenn GM, et al. BHD mutations, clinical and molecular genetic investigations of Birt-Hogg-Dubé syndrome: a new series of 50 families and a review of published reports. J Med Genet 2008;45:321-331.
Shchelochkov OA, Cheung SW, Lupski JR, et al. Genomic and clinical characteristics of microduplications in chromosome 17. Am J Med Genet A 2010;152A:1101-10.
Li J, Liu F, Liu X, et al. Heterozygous germline FLCN mutation in Birt-Hogg-Dubé syndrome with bilateral renal hybrid oncocytic/chromophobe tumor and unilateral renal chromophobe cell carcinoma: a case report. J Cancer Res Clin Oncol 2023;149:2319-25.
Ray A, Chattopadhyay E, Singh R, et al. Genetic insight into Birt-Hogg-Dubé syndrome in Indian patients reveals novel mutations at FLCN. Orphanet J Rare Dis 2022;17:176.
Menko FH, van Steensel MA, Giraud S, eta al.European BHD Consortium. Birt-Hogg-Dubé syndrome: diagnosis and management. Lancet Oncol 2009;10:1199-206.
Sattler EC, Steinlein OK. Birt-Hogg-Dubé Syndrome. 2006 Feb 27 [Updated 2020 Jan 30]. In: Adam MP, Feldman J, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2024.
Wataya-Kaneda M, Tanaka M, Hamasaki T, Katayama I. Trends in the prevalence of tuberous sclerosis complex manifestations: an epidemiological study of 166 Japanese patients. PLoS One 2013;8:e63910.
Teng JM, Cowen EW, Wataya-Kaneda M, et al. Dermatologic and dental aspects of the 2012 International Tuberous Sclerosis Complex Consensus Statements. JAMA Dermatol 2014;150:1095-101.
Schmidt LS, Linehan WM. FLCN: The causative gene for Birt-Hogg-Dubé syndrome. Gene 2018;640:28-42.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Thai Journal of Dermatology

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
เนื้อหาและข้อมูลในบทความที่ลงตีพิมพ์ในวารสารโรคผิวหนัง ถือเป็นข้อคิดเห็นและความรับผิดชอบของผู้เขียนบทความโดยตรงซึ่งกองบรรณาธิการวารสาร ไม่จำเป็นต้องเห็นด้วย หรือร่วมรับผิดชอบใดๆ
บทความ ข้อมูล เนื้อหา รูปภาพ ฯลฯ ที่ได้รับการตีพิมพ์ในวารสารโรคผิวหนัง ถือเป็นลิขสิทธิ์ของวารสารฯ หากบุคคลหรือหน่วยงานใดต้องการนำทั้งหมดหรือส่วนหนึ่งส่วนใดไปเผยแพร่ต่อหรือเพื่อกระทำการใดๆ จะต้องได้รับอนุญาตเป็นลายลักอักษรจากบรรณาธิการวารสารโรคผิวหนังก่อนเท่านั้น


