Determination of patient doses in 2D and 3D mammography at Udonthani Cancer Hospital
Keywords:
Breast Cancer Screeninng, Radiation Dose, Mammography, Digital Mammography TomosynthesisAbstract
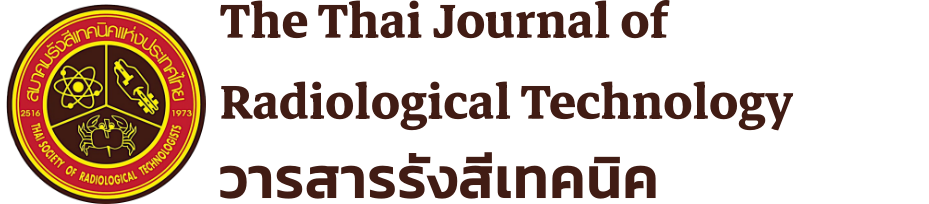
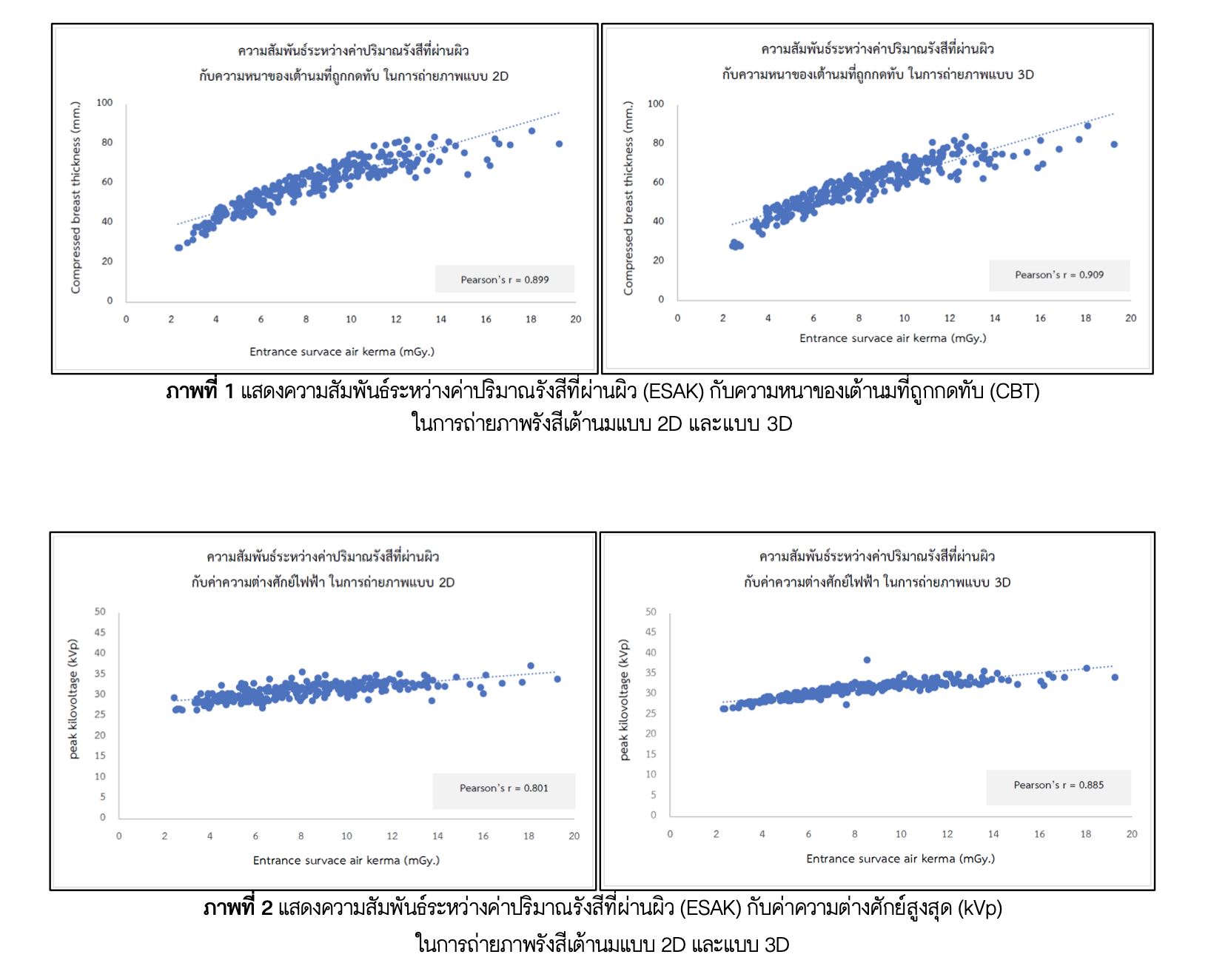
Background: Mammography examination is commonly used for the breast cancer screening. Since the radiation dose is contributed to the patient breast tissues, we should monitor and control the radiation dose within the international standard level. This study aimed to determine the radiation doses obtained from 2D and 3D mammography at Udonthani Cancer Hospital (UDCH). Methods: Retrospective data of 280 Thai women patients who have age greater than 40 years-old with body weight range 40-70 kg were randomly collected from the database system of UDCH between January and December 2019. Mean glandular dose (MGD) and its related parameters were analyzed using the descriptive statistics and Pearson’s correlation coefficient. Results: The results showed that the median values of MGD of craniocaudal views (CC) was 1.74 mGy and mediolateral oblique view (MLO) was 2.01 mGy from 2D and 3D mammographic examinations of CC views was 2.09 mGy and MLO was 2.34 mGy. Three related parameters that affected the MGD were tube current-time (mAs), compressed breast thickness and peak kilovoltage (kVp), respectively. There was slightly different of MGD between the right and left side of breast. Conclusion: The radiation doses obtained from the mammography examinations in this study was lower than the Thailand national diagnostic reference levels that published in 2021, which is appropriate for the patients. Notwithstanding, the radiologic technologist should monitor and verify the radiation dose regularly for the patients.
Downloads
References
2. American college of radiology. Mammography quality control manual mammography phantom image quality evaluation, 1999.
3. Kanal KM, Krupinski E, Berns EA, Geiser WR, Karellas A, Mainiero MB, et al. ACR-AAPM-SIIM Practice Buideline for Determinants of Image Quality in Digital Mammography. J Digital Imaging 2013; 26: 10-25.
4. IAEA Safety Series No. 115. International Basic Safety Standards for Protection against Ionizing Radiation and for the Safety of Radiation Sources. Vienna: International Atomic Energy Agency, 1994.
5. Xiang Du, Ningle Yu, Yimei Zhang, Jin Wang. The relationship of the mean glandular dose with compressed breast thickness in mammography. J Public Health Emerg 2017; 1:32.
6. Prachumporn P, Eimorn M, Pattaraporn D. Mammographic Technique from Mammography. Srinagarind Med J 2008; 23(1).
7. Kanlayanee T, Anchali K. Radiation dose from digital breast tomosynthesis system. Chula Med J 2014 May-Jun; 58(3): 235-45.
8. Prissana T, Jiraporn S, Amornrat M. Radiation dose from digital mammography in Srinagarind Hospital. Srinagarind Med J 2015; 30(6):604-608.
9. Chatsuda S, Kamonchanok M, Khonpat P. Local diagnostic reference levels for breast screening using digital mammography at Tanyawaj Breast Center, Songklanagarind Hospital. Thai J Rad Tech 2019; 44(1): 1-7.
10. Hinkle, D.E, William, W. and Stephen G. J. Applied statistics for the behavior sciences. 4thed. New York: Houghton Mifflin,1998.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 The Thai Society of Radiological Technologists

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
บทความที่ได้รับการตีพิมพ์เป็นลิขสิทธิ์ของสมาคมรังสีเทคนิคแห่งประเทศไทย (The Thai Society of Radiological Technologists)
ข้อความที่ปรากฏในบทความแต่ละเรื่องในวารสารวิชาการเล่มนี้เป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับสมาคมรังสีเทคนิคแห่งประเทศไทยและบุคคลากรท่านอื่น ๆในสมาคม ฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใดๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเองแต่ผู้เดียว