Innovation of inexpensive customized bolus in radiotherapy from 3D printer using silicone bolus
Keywords:
Silicone bolus, Dose attenuation, Surface dose, 3D PrinterAbstract
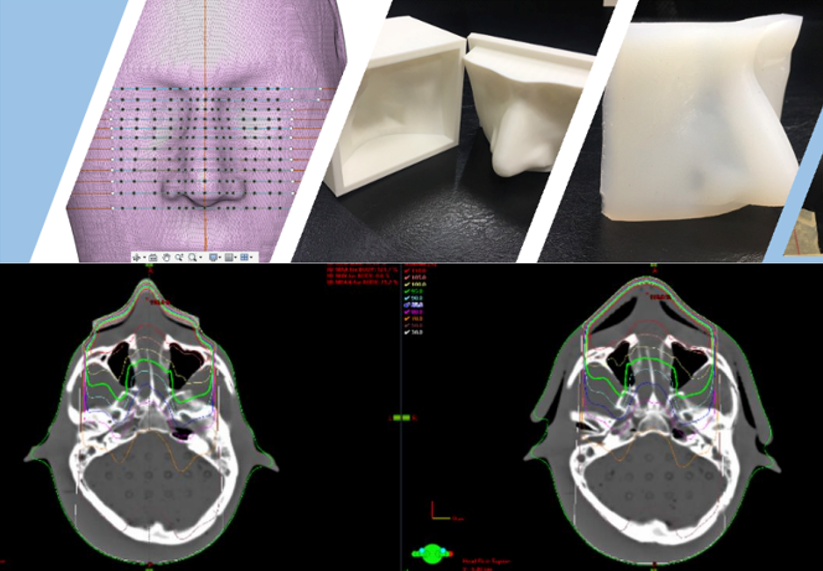
Introduction: Bolus is a water-equivalent material that is commonly used to increase the buildup region dose and compensate for missing tissue in radiotherapy. The commercial superflab bolus is quite expensive and cannot perform the perfect contact with the irregular shape of the patient’s surface. The aim of this study was to study the characteristics of in-house silicone rubber bolus to apply in radiotherapy. Methods: The methods start with mixing the RA-00A and RA-00B solutions into a homogeneous substance. The solutions were poured into the holder to create a 1 cm silicone rubber thickness with the size of 30x30 cm2. The physical properties of thickness, density, and hardness were evaluated and compared with the commercial bolus. A piece of silicone rubber bolus was scanned by a CT simulator. The CT images of the silicone rubber bolus were used to evaluate the Hounsfield unit (HU) and the dose attenuation was also evaluated in the Eclipse treatment planning system. The 3D shape of the nose was created as a 3D customized bolus using 3D printed technology. Results: We found that the commercial bolus and the customized one showed a thickness of 1.05±0.00 cm and 1.07±0.01 cm, density of 1.03 and 0.99 g/cm3, and hardness of 2.5 HA and 1.5 HA, respectively. The HU of commercial bolus and customized bolus were -124±63.3 and -73±42.5, respectively. The surface dose differences between silicone bolus and commercial bolus of 6 MV, 10 MV, 6 MeV, and 9 MeV were 0.4%, 0.9%, 0.7%, and -0.4%, respectively. The silicone bolus can increase surface doses in clinics of 68.5%, 67.1%, 17.7%, and 7.4% compared to the amount of radiation at the surface without the bolus, it will be 30,23.1,81.5, and 86.9 for 6 MV, 10 MV, 6 MeV, and 9 MeV, respectively. comparable to the result from a commercial superflab bolus. The 3D customized bolus presented the perfect fit to the irregular surface shape phantom and significantly increased the buildup region dose. Conclusion: Silicone rubber is an alternative material that can replace commercial bolus because of the comparable properties with more than 20 times cheaper prices. It can also be molded into 3D shapes according to organs and lesions.
Downloads
References
Podgorsak EB. Radiation oncology physics: a handbook for teacher and students. Vienna: International Atomic Energy Agency.
Gunhan B, Kemikler G, Koca A. Determination of surface dose and the effect of bolus to surface dose in electron beams. Med Dos. 2003;28:193-8.
Wong G, Lam E, Bosnic S, et al. Quantitative effect of bolus on skin dose in postmastectomy radiation therapy. Research. 2020;51:462-9.
Lu Y, Song J, Yao X, An M, Shi Q, Huang X. 3D printing polymer-based bolus used for radiotherapy. Int J Bioprint. 2021;7:27-42.
Gong P, Dai G, Wu X, et al. Application of thermoplastic elastomer (TPE) bolus in postmastectomy radiotherapy. The Breast. 2022;66:317-23.
Chaloeiparb C, Wiriyatharakij T, Apipanyasopon L. Formation and surface dose determination of natural rubber bolus for a 9-MeV therapeutic electron beam. J Th Asso Rad Oncol. 2020;26:R55-67.
Sutanto H, Marhaendrajaya I, Wiratma G, et al. The properties of bolus material using silicone rubber. IOP Conf. Series: Mater Sci Eng. 2019;622:012002.
Butson MJ, Cheung T, Yu P, et al. Effects on skin dose from unwanted air gaps under bolus in photon beam radiotherapy. Radiat Meas. 2000;32:201-4.
Kong M, Holloway L. An investigation of central axis depth dose distribution perturbation due to an air gap between patient and bolus for electron beams. Australas Phys Eng Sci Med. 2007;30:111-9.
Wang KM, Rickards A, Bingham T, Tward JD, Price RG, Technical note: Evaluation of a silicone-based custom bolus for radiation therapy of a superficial pelvic tumor. J Appl Clin Med Phys.2022;23:e13538.
Fujimoto K, Shiinoki T, Yuasa Y, et al. Efficacy of patient‐specific bolus created using three‐dimensional printing technique in photon radiotherapy. Phys Med. 2017;38:1-9.
Zhang C, Lewin W, Cullen A, Thommen D, Hill R. Evaluation of 3D-printed bolus for radiotherapy using megavoltage X-ray beams. Rad Phys Tech. 2023;16:1-8.
Wang X, Wang X, Xiang Z, et al. The clinical application of 3D-printed boluses in superficial tumor radiotherapy. Front Oncol. 2021;11:698773.
Yu S, Ahn SH, Choi SH, Ahn WS, Jung IH. Clinical application of a customized 3D-printed bolus in radiation therapy for distal extremities. Life. 2023;13:362-70.
Biltekin F, Yazici G, Ozyigit G. Characterization of 3D-printed bolus produced at different printing parameters. Med Dos. 2021;46:157-163.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Thai Society of Radiological Technologists

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
บทความที่ได้รับการตีพิมพ์เป็นลิขสิทธิ์ของสมาคมรังสีเทคนิคแห่งประเทศไทย (The Thai Society of Radiological Technologists)
ข้อความที่ปรากฏในบทความแต่ละเรื่องในวารสารวิชาการเล่มนี้เป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับสมาคมรังสีเทคนิคแห่งประเทศไทยและบุคคลากรท่านอื่น ๆในสมาคม ฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใดๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเองแต่ผู้เดียว